Health Care Access & Coverage | Health Equity
Blog Post
A Cautionary Tale About Medicaid Work Requirements
Historical analysis of welfare requirements show large spillover effects
In a new paper in JAMA Network Open, our team looked at the potential effects of Medicaid work requirements on Medicaid participation among those not actually subject to these requirements. We estimate that these “spillover effects” – which thus far have not been part of the conversation on work requirements – could be quite large. How we arrived at this answer is worth a bit of explanation.
Nearly three years ago, we were hired to independently evaluate Kentucky’s proposed Section 1115 Medicaid waiver, which included work requirements. While creating our study design, we thought about the total effects of work requirements on Medicaid participation. We wondered if imposing work requirements – which focused specifically on those considered “able-bodied” – might have spillover effects on Medicaid participation among people who wouldn’t be subject to them.
Why might this happen? Complex changes to benefit programs may create confusion among would-be participants and the staff helping administer those benefits. Work requirements may also stigmatize participation or make benefits seem more out of reach. There is a pretty large literature suggesting that these spillover effects are meaningful and important to capture. A lot of this evidence comes from the welfare reform era. For example, the transition from the Aid to Families with Dependent Children (AFDC) program to the Temporary Assistance for Needy Families (TANF) program – which included imposition of work requirements – was associated with meaningful reductions in participation in programs like Medicaid. Our team wanted to study whether this spillover phenomenon applied to Medicaid work requirements. Namely, could implementing a work requirement among one group of Medicaid beneficiaries impact participation among another unaffected group of beneficiaries?
Work requirements were still very new when we were designing our study, and so we needed to turn to history. Thanks to Kristen Underhill, our Co-PI and resident legal expert, we found out that a handful of states had enacted a de facto Medicaid work requirement as part of welfare reform. Basically, the states shown in the map in Figure 1, as of 2000, included termination of Medicaid as a sanction for not complying with new welfare work requirements.
Critically, these sanctions only applied to TANF beneficiaries. To look at spillovers, we examined whether their implementation affected Medicaid participation among those unlikely to receive TANF. Specifically, we used a difference-in-differences research design, which allowed us to compare changes in Medicaid participation among low-income adults in states implementing sanctions versus the same changes for low-income adults in states not implementing sanctions. Our models accounted for baseline differences across state, national secular trends in Medicaid participation, unemployment rates (since the economy was improving over most of the study period), the imposition of other types of TANF sanctions, and Medicaid eligibility thresholds.
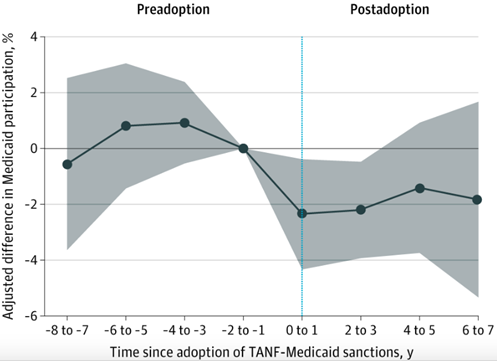
We found that low-income adults living states with Medicaid sanctions for failing to meet TANF work requirements, but not subject to these requirements, were less likely to report Medicaid participation in the year after implementation. The effect size, as shown in Figure 2, amounts to a 10% decrease in Medicaid participation rates.
Key Takeaways
Our results have a number of important implications. Here are some takeaways:
- The spillover effects of Medicaid work requirements could be large. The 10% relative decline is almost half of the estimated 1-year direct effect of the recent Arkansas work requirement program.
- While this is a historical piece, confusion around eligibility and rules seen in modern work requirement programs suggest that these spillovers may be salient today.
- Potential spillover effects would compound concerns around accurate targeting of work requirements. It is very difficult to accurately ascertain who meet exemptions to work requirements and who do not – and that’s just among beneficiaries would might be subject to them.
- There are many implications of our findings for COVID-19. Efforts to tighten social programs among some groups may inadvertently reduce participation among other groups. Making programs more accessible for those in need, particularly during these unprecedented times, may require (among other things) dramatically simplifying rules.
The article, “Association Between State Policies Using Medicaid Exclusions to Sanction Noncompliance With Welfare Work Requirements and Medicaid Participation Among Low-Income Adults,” was published in JAMA Network Open on May 11, 2020. Authors include Atheendar S. Venkataramani, MD, PhD; Elizabeth F. Bair, MS; Erica Dixon, PhD; Kristin A. Linn, PhD; William J. Ferrell, MPH; Kevin G. Volpp, MD, PhD; and Kristen Underhill, JD, DPhil.