Health Care Access & Coverage
Brief
Effects of the ACA on Health Care Cost Containment
What has the ACA done to "bend the cost curve"? Fourth and Final in a Series on the Impact of the ACA

Summary
This brief reviews the evidence on how key ACA provisions have affected the growth of health care costs. Coverage expansions produced a predictable jump in health care spending, amidst a slowdown that began a decade ago. Although we have not returned to the double-digit increases of the past, the authors find little evidence that ACA cost containment provisions produced changes necessary to “bend the cost curve.” Cost control will likely play a prominent role in the next round of health reform and will be critical to sustaining coverage gains in the long term.
While the Affordable Care Act (ACA) has been largely defined by its coverage expansions, its authors recognized the need to include mechanisms to slow the growth of health care costs. The law’s provisions took aim at Medicare spending and to a lesser extent, factors that affect costs in the individual and group private market. To understand the law’s impact and potential to “bend the cost curve,” it is important to isolate the effects of the ACA from those attributable to the economic recession and recovery. Although the ACA’s future is in doubt, cost containment will remain a key ingredient of any health reform effort. In this brief, we discuss key ACA provisions and their effects on containing overall cost growth and the cost of ACA-related gains in coverage.
The Trajectory of National Health Spending
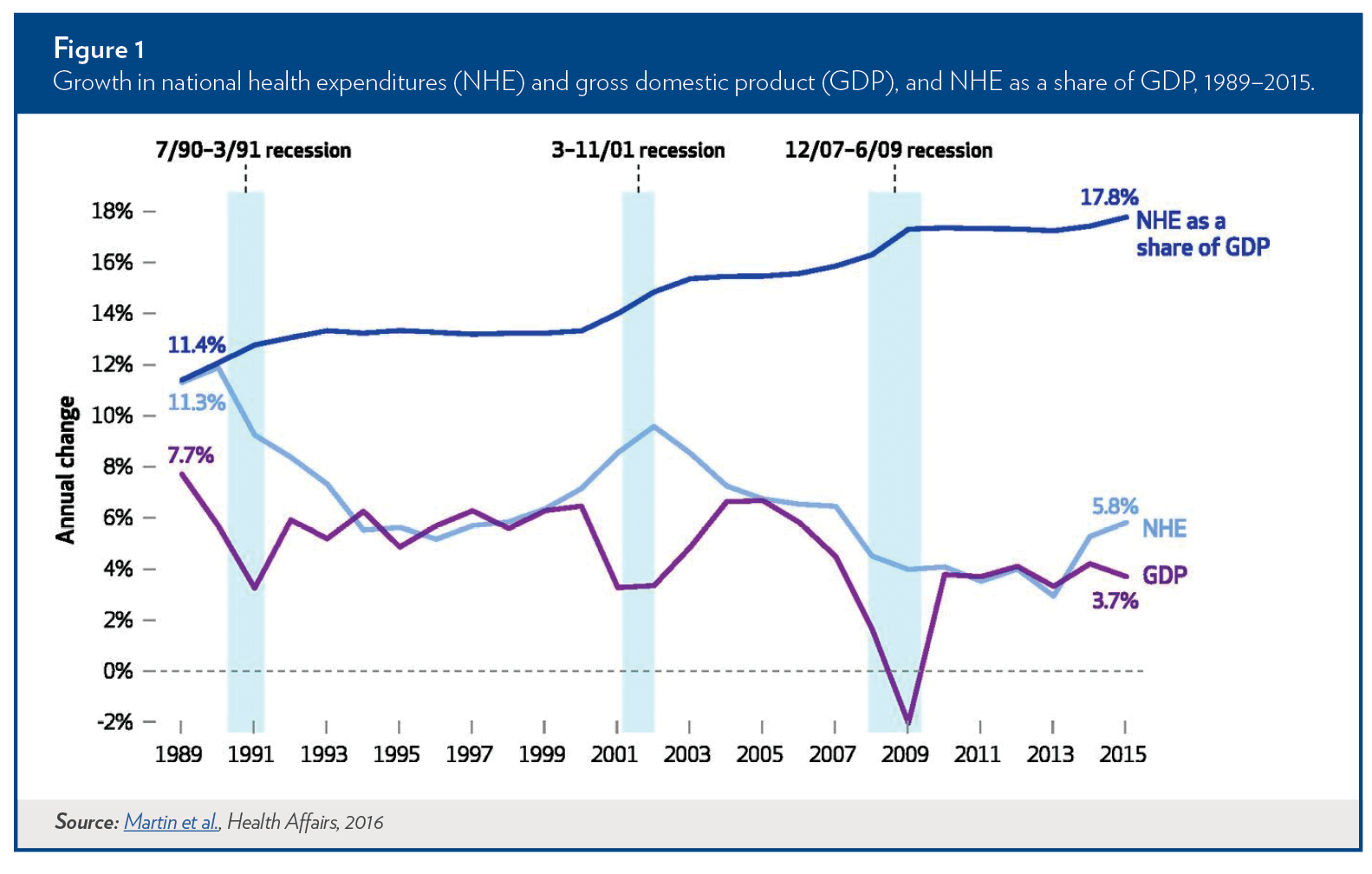
First, let’s look at the big picture. As shown, national health expenditure (NHE) grows regardless of macroeconomic conditions, although this growth often slows in periods of recession. The historical patterns reflect slower growth due to cost containment efforts of managed care in the 1990s; upturns from the managed care backlash and spending on blockbuster drugs in the early 2000s; a deceleration through 2007 with a rapid rise of cheaper generic drugs and slower rate of introduction of new technology; and a dramatic slowdown in growth through 2013, with a deep recession and modest recovery. The patterns also reflect the impact of the ACA, as large-scale coverage expansions began in 2014.
Why the dramatic slowdown from 2007-2013? Studies estimate that the 2007-2009 recession and the slow recovery from it explained somewhere between 37 percent and 70 percent of the slowdown. Others point to the spread of high-deductible health plans (HDHPs), which incentivize price-conscious consumers to shop for care and avoid low value care. Just four percent of employers offered HDHPs in 2005; by 2011, nearly a third of employers offered such plans. A 2013 study suggested that less generous benefit design might have accounted for 20 percent of the slowdown. Slower adoption of expensive new medical technology and fewer new blockbuster drugs may have also been contributing factors.
The ACA’s coverage expansion in 2014 spurred a spike in spending, as would be expected. These provisions allowed millions of people to get health insurance through the exchanges and through Medicaid expansion. Health care costs increased by 5.3 percent in 2014, from a low of 2.9 percent in 2013. The Office of the CMS Actuary estimated that increased use of health care services accounted for nearly 40 percent of the increase in per-capita health spending. Health costs grew by 5.8 percent in 2015, and preliminary estimates by the Altarum Institute indicate a steady growth rate of 5.4 percent over 2015.
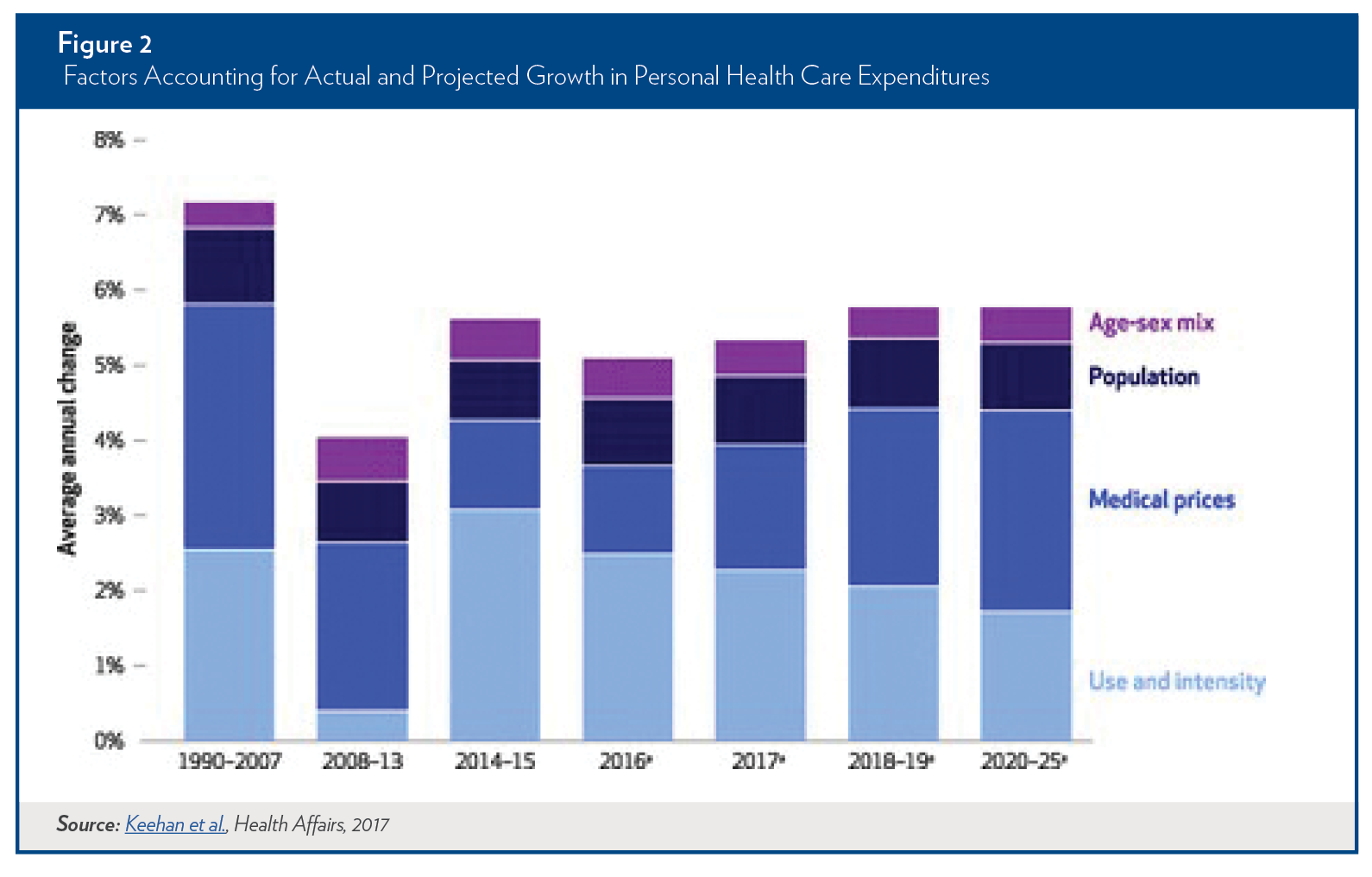
Analysis of the ACA’s effects on cost containment rests on three concepts: first, that any provisions affecting only the individual market can have little effect on overall health spending, because only 6% of people under age 65 are in that market; second, that the slowing of the trajectory of health care spending predates the ACA and complicates analysis of its effects; and third, that while increased utilization of health care due to the ACA’s coverage expansion drove cost growth in the early years, health care prices will likely exert a powerful influence on the trajectory of health care costs over the long run.
This point is brought home in a new analysis by the Office of the CMS Actuary, which projects that medical prices will account for an increasing share of cost growth as use and intensity of services decelerate, possibly due to meeting pent-up demand (Figure 2.)
In the following sections, we review key provisions in the ACA that target cost containment and what we know about their effects.
Key Cost-Containment Provisions
Medicare Reforms
One of the most immediate and direct ways that the ACA produced savings was through reductions in provider payment updates and Medicare Advantage (MA) payments. Prior to the ACA, payments to MA plans were 14 percent higher than the cost of covering similar beneficiaries under the traditional Medicare program, according to the Medicare Payment Advisory Commission. The ACA reduced payments to MA plans over six years, and by 2016, payments to MA plans were just two percent higher than costs in the traditional Medicare program. Although critics were concerned that these cuts would mean that plans withdrew from the program, according to Kaiser Family Foundation, enrollment actually increased from 24 percent in 2009 to 31 percent in 2016. The payment reductions produced short-term federal savings of $68 billion between 2011 and 2016.
The ACA provided a regulatory framework for containing costs in Medicare by setting a per capita target for spending growth and creating a 15-member Independent Payment Advisory Board (IPAB) to develop a plan to reduce spending if that target is exceeded. What the board can recommend is constrained: by law, it cannot raise premiums, reduce benefits, or increase cost sharing, meaning that their recommendations are mostly confined to cuts in provider payments. The board’s proposals become law unless Congress explicitly overrides them. Spending did not exceed per capita targets in the ACA’s first three years, and therefore IPAB was not triggered. The IPAB currently has no members, which reflects a congressional majority strongly opposed to its existence. IPAB has been targeted for repeal on a bipartisan basis and is not likely to survive as a cost containment mechanism.
Beyond IPAB, the ACA authorized multiple initiatives designed to wring savings out of Medicare through administrative simplification, improved quality, better care coordination, and reduced payment rates. Some of the most prominent examples include the Hospital Readmissions Reduction Program (HRRP); Accountable Care Organizations (ACOs) through the Medicare Shared Savings Program and Pioneer Program; primary care medical homes; and bundled payment models. This emphasis on moving to value-based reimbursement dovetails with changes in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), which mandated that Medicare move from fee-for-service to alternative payment models, such as those with risk-sharing arrangements or reimbursement tied to quality measures.
Early evidence from the HRRP has shown decreases in hospital readmissions, but no firm data on overall cost savings. According to an analysis by the Kaiser Family Foundation, for fiscal year 2017, 79 percent of hospitals in the United States will receive a penalty and that penalty payments will total over half a billion dollars.
Most of the ACA’s provisions promoting value-based payment were small-scale, voluntary programs that, at best, can be considered proof-of-concept demonstrations rather than cost containment initiatives. The programs have had variable effects on costs, and their ability to “bend the cost curve” remains conjecture.
For example, the ACA promoted ACOs as both a quality improvement and cost containment mechanism. In 2015, more than 400 ACOs in the Pioneer ACO Model and the Medicare Shared Savings Program generated $429 million in savings, but bonuses paid to high-performing ACOs produced a net loss of $216 million. ACOs with more experience tend to perform better over time.
A recent study of the Comprehensive Primary Care Initiative (CPCI), a 2012 CMS initiative in 500 practices to improve quality and reduce costs, found minimal effects on costs or outcomes after two years. The program did not generate enough savings in Medicare Parts A and B to cover care-management fees associated with the program.
In the most recent CMS evaluation, bundled payments also show modest effects on costs, depending on the model and clinical condition. In the most prevalent model, episode payments decreased spending for orthopedic surgery (mostly hip and knee replacements), but increased spending for spinal surgery, relative to comparison hospitals. These results were from voluntary programs; although CMS issued rules for a mandatory bundled payment system for heart attack treatment, bypass surgery, and surgical hip and femur fracture treatment in December 2016, the mandatory system may not survive a Republican administration and Congress that is opposed to it.
Private Market Insurance Reforms
The ACA includes a slew of new regulations affecting the private insurance market, both on and off the exchanges. These include a prohibition on lifetime and annual caps on coverage, a mandate to cover “essential health benefits,” premium rate review, and the Medical Loss Ratio (MLR) provision, which required insurers to provide a customer rebate if they spend too high a percentage of premium dollars on non-medical expenditures. It is difficult to tease out the countervailing effects of these regulations on health care costs, especially because the provisions affect the individual, small group, and large group markets differently.
The most significant provision targeting long-term cost growth is the tax on high-cost health plans, known as the “Cadillac Tax”. The provision imposes a 40 percent excise tax on high-cost, employer-sponsored insurance that was to begin in 2018. However, Congress voted to delay its implementation until 2020—an indication of the political difficulties of reining in health spending. Proponents predicted that this tax would spur employers to shift away from high-cost health insurance—long incentivized by preferential tax treatment—and in so doing drive down overall health care spending. Many unions, employer groups, and insurers continue to oppose the tax, however, and it remains unclear whether Congress will allow it to take effect.
In the individual market, the ACA focused on the creation and stability of exchanges as a way to promote competition and contain health care costs. Economic theory predicts, and evidence suggests, that a higher number of insurers in a marketplace correlates with lower premiums. But as we stated in a previous brief in this series, the exchanges have undergone significant turmoil in the past three years, and recent insurer departures have left some marketplaces with little or no competition.
In the individual market, premium rate reviews were an explicit mechanism to restrain premium increases and keep costs down. An early analysis by Kaiser Family Foundation of the rate review provision found that 20 percent of filings resulted in lower premium increases due to the rate review process. On average, premium rate increases were 1.4 percentage points lower than originally requested. Another analysis by the Department of Health and Human Services found that in 2013, rate review reduced premiums in the individual and small-group markets by almost $1 billion. The actual effects on health care costs, however, is unknown, given that insurers could have inflated premium increase requests above what would have been present in the absence of the provision.
Commonwealth Fund data on the effects of the medical loss ratio provision show that the law has had a modest effect on reducing premium overhead and providing consumer rebates. Insurers reduced overhead spending by $350 million in 2011 and $1 billion in both 2012 and 2013. According to the Congressional Budget Office (CBO), rebates to customers, effectively lowering their premiums, totaled over $2.4 billion over the 2011 – 2014 period. The overall impact of the MLR provision on costs is uncertain, as insurers can reduce administrative costs or increase claims costs to avoid paying penalties.
Where We Are and What We Don’t Know
Much is unknown about the effects of various cost-containment provisions within the ACA. Depending on whether the ACA is repealed in total or pieces of it remain, we may not be able to determine what effects the law has had. To date, evidence has shown health spending has slowed since the ACA’s passage in 2010. However, as ACA coverage expansion provisions are implemented, we are seeing an increase in overall spending, although to an extent, that is to be expected. Medicare demonstrations around payment and delivery reforms are potentially useful in slowing cost growth, but they remain unproven and even the successful programs produce only modest savings. In private insurance, provisions like rate review and MLR have had, at most, a minimal impact on overall health care costs.
Outside of the ACA explicitly, high-deductible health plans and insurance mergers will likely have important effects on health spending, although the magnitude is hard to predict. Also in the mix are the long-term effects of changes in Medicare (particularly the role of IPAB), the Cadillac Tax, and the role of new technologies.
Medicare. In 2015, the CMS Chief Actuary found that that Medicare per-capita spending growth was just 0.12 percentage points below the trigger rate for IPAB to take effect. It is likely that the IPAB threshold of GDP + one percentage point will be hit in 2017. Although it is highly unlikely that IPAB will survive, any mechanism that caps spending at this rate would force billions of dollars in savings.
Cadillac Tax. The provision most likely to have a dramatic effect on premiums and curbing spending growth—the Cadillac Tax—remains years from implementation in the best-case scenario. Estimates of its explicit effects are varied. CBO and the Joint Committee on Taxation (JCT) recently estimated that in 2020, even if employers did not make any changes in response to the tax, five to ten percent of enrollees in ESI plans would be subject to the tax and that share would grow to between 15 and 20 percent in 2025. If implemented as currently outlined under the law, CBO and JCT estimate that the tax will reduce deficits by nearly $80 billion by 2026.
Some changes have occurred even though the tax has not been implemented. The 2016 Kaiser Employer Health Benefits Survey found that some employers have changed their plans’ coverage or increased cost sharing to avoid the tax. Another survey done by Mercer found that a significant number of respondents were taking steps that will limit their exposure to the tax. Forty-eight percent have implemented a consumer-directed health plan (CDHP), 38 percent have encouraged employees into CDHPs, 28 percent raised deductibles, and 17 percent dropped high-cost plans. A recent study found that consumer-directed health plans—combining high deductible plans with personal medical accounts—reduced health care spending significantly for firms offering CDHPs over three years.
Technology. The role of technology in accelerating health spending has been well established. While we do not know what new technologies are on the horizon, the current growth and proliferation of specialty drugs and new drug price increases suggest upward pressure will be exerted. New technologies can extend treatments to broader populations and improve life expectancy. They also can change the cost of treating patients, potentially increasing cost by providing more services, having a negligible effect through replacement, or decreasing utilization and potentially cost. The key challenge for policymakers is designing systems that promote cost-effective technologies while reducing the use of expensive technologies that do little to improve outcomes.
Policy Considerations Moving Forward
It is too early to draw firm conclusions about the ACA’s effect on cost containment, especially given that the provisions with the greatest potential impact— notably the Cadillac Tax and the IPAB —have not been implemented. Still, the intense opposition to both provisions provides good reason to temper our expectations about the degree of cost containment we can achieve through the ACA alone. As the Trump Administration and Republican controlled Congress debate repealing or replacing the ACA, policymakers face a number of choices to reduce the growth of health care costs going forward.
IPAB, as designed, has few proponents. In a comprehensive report, the Kaiser Family Foundation list a number of options for amending IPAB. These include modification to spending target and limits on savings targets, revising IPAB and Congressional consideration of proposals, and revising the scope of recommendations. But the idea of a per capita Medicare cap as a failsafe or backstop measure to contain costs remains on the table.
The Cadillac Tax incorporated a generally accepted economic principle—that preferential tax treatment encourages overconsumption of health care—in what appears to be a politically unacceptable way. Options to achieve the shared goals of the Cadillac Tax or make the tax more equitable could include a cap on the tax exclusion of health benefits, changing thresholds and indexing, and phasing in the tax over different income tiers.
The climate for Congressional action on drug prices could dampen the impact of these technologies on overall health spending, although policy has proven difficult to enact in this area. Interventions aimed at reducing drug spending range from allowing the government to negotiate drug pricing, prohibit “pay for delay” arrangements, to allowing imported drugs from outside the United States. The recently passed 21st Century Cures Act will increase research funding and eventually lead to the development of more expensive new drugs, exerting upward pressure on overall health spending.
The long-term impact of the ACA on health care costs depends on several factors, chief among them whether the law is repealed or stripped down to its bare bones. If Congress continues to punt on the Cadillac Tax and repeals IPAB, the prospect of future cost containment may be bleak. Long-term trends in medical technology and new pharmaceuticals remain important unknowns, but the ACA does little to directly affect these drivers of health care cost growth. The ACA-driven payment and delivery innovations have thus far yielded modest cost savings. Ongoing trends in the employer market, such as the move toward consumer-directed health plans, might hold the most promise in the absence of more directed government policies.
The challenge to “bend the cost curve” remains an urgent one. The ACA provided needed coverage for millions of previously uninsured people, without a return to the double-digit spending increases of the past. But the sustainability of these coverage gains, and extensions to the remaining uninsured, likely depend on implementation of cost containment measures that more directly, and forcefully, produce long-term changes in the growth of health care costs.
References
Baker, L., Birnbaum, H., Geppert, J., Mishol, D. & Moyneur, E. (2003). The relationship between technology availability and health care spending. Health Affair. Retrieved from http://content.healthaffairs.org/content/early/2003/11/05/hlthaff.w3.537.long
Chandra, A. & Skinner, J. (2012). Technology growth and expenditure growth in healthcare. Journal of Economic Literature, 50(3), 654-80. Retrieved from https://www.aeaweb.org/articles?id=10.1257/jel.50.3.645
Chandra, A., Holmes, J., & Skinner, J. (2013). Is this time different? The slowdown in healthcare spending. The National Bureau of Economic Research. Retrieved from http://www.nber.org/papers/w19700
Cutler, D., & Sahni, N. R. (2013). If slow rate of health care spending growth persists, projections may be off by $770 billion. Health Affairs, 32(5), 841-850. Retrieved from http://content.healthaffairs.org/content/33/8/1399.abstract
Dafny, L., Gruber, J. & Ody, C. (2015). More insurers lower premiums: evidence from initial pricing in the health insurance marketplaces. American Journal of Health Economics, 1(1), 53-81. Retrieved from http://www.mitpressjournals.org/doi/10.1162/AJHE_a_00003#.WK8mJFXyu71
Dale, S.B., Ghosh, A., Peikes, D.N., Day, T.J., Yoon, F.B., Taylor, E.F., … Brown, R. (2016). Two-year costs and quality in the Comprehensive Primary Care Initiative. The New England Journal of Medicine, 374, 2345-2356. Retrieved from http://www.nejm.org/doi/ref/10.1056/NEJMsa1414953#t=abstract
Dranove, D., Garthwaite, C., & Ody, C. (2014). Health spending slowdown is mostly due to economic factors, not structural change in the health care sector. Health Affairs, 33(8), 1399-1406. Retrieved from http://content.healthaffairs.org/content/33/8/1399.abstract
Haviland, A.M., Eisenberg, M.D., Mehrota, A., Huckfedlt, P.J., & Sood, N. (2015). Do “consumder-directed” health plans bend the cost curve over time? The National Bureau of Economic Research. Retrieved from http://www.nber.org/papers/w21031
Keehan, S.P., Stone, D.A., Poisal, J.A., Cuckler, G.A., Sisko, A.M., Smith, S.D., … Lizonitz, J.M. (2017). National health expenditure projections, 2016-25: price increases, aging push sector to 20 percent of economy. Health Affairs. Retrieved from http://content.healthaffairs.org/content/early/2017/02/14/hlthaff.2016.1627
Martin, A. B., Hartman, M., Washington, B., Catlin, A., the National Health Expenditure Accounts Team. (2016). National health spending: faster growth in 2015 as coverage expands and utilization increases. Health Affairs. Retrieved from http://content.healthaffairs.org/content/early/2016/11/22/hlthaff.2016.1330.full
Muhlestein, D., Saunders, R. & McClellan, M. (2016). Medicare Accountable Care Organization results from 2015: the journey to better quality and lower costs continues. Health Affairs Blog. Retrieved from http://healthaffairs.org/blog/2016/09/09/medicare-accountable-care-organization-results-for-2015-the-journey-to-better-quality-and-lower-costs-continues/
Ryu, A.J., Gibson, T.B., McKellar, M.R., & Chernew, M.E. (2013). The slowdown in health care spending in 2009-11 reflected factors other than the weak economy and thus may persist. Health Affairs, 32(5), 835-840. Retrieved from http://content.healthaffairs.org/content/32/5/835.abstract