
Methadone Use Rises—But Too Few People Get Opioid Medication
Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
Blog Post
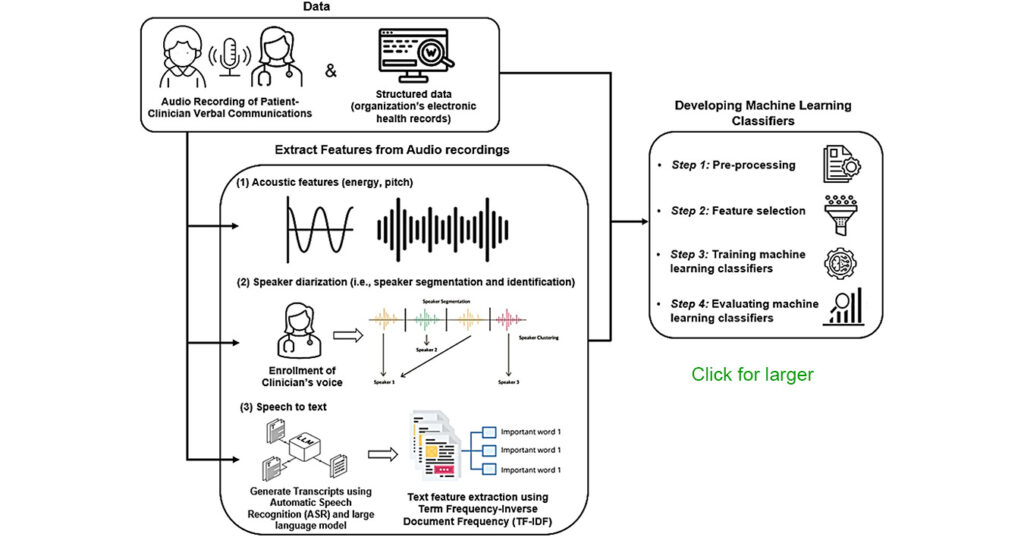
A new study suggests artificial intelligence (AI) may help clinicians identify which seriously ill patients are ready for palliative care — by analyzing the energy, pitch, and other subtle vocal cues in recorded group phone conversations among patients, caregivers, and health care providers.
The new work by a team led by LDI Senior Fellow and Penn Nursing School Assistant Professor Jiyoun Song, PhD, APRN, is the first to use speech processing to identify palliative care preferences during discussions and decision-making in managed long-term care (MLTC), a type of Medicaid-managed care for community-dwelling patients that need home and community-based services.

Titled “Leveraging Patient and Surrogate Caregiver Communication With Clinicians to Predict Palliative Care Decisions: A Speech Processing Study,” the new study was published in the March 2026 edition of Geriatric Nursing.
The project used automated speech processing to extract acoustic features from conversations, including energy, pitch, and pauses, combining those with text from transcripts and demographic and clinical data. Multiple AI models were tested to predict whether patients would accept or refuse palliative care. The best-performing model correctly classified about two-thirds of conversations — a modest result that researchers describe as an early proof of concept rather than a tool ready for clinical use.
It is the latest in a broad set of health care industry efforts — from structured communication training and embedded advance care planning to AI systems that analyze electronic health records to predict short-term mortality — aimed at addressing a persistent problem in care for seriously ill older adults: Clinicians often postpone palliative care discussions, and patients’ wishes frequently go undocumented or are lost across care settings.
The New England Journal of Medicine Catalyst Insights Council has reported that roughly 60 percent of the people who need palliative care in the U.S. do not get it. “Palliative care” refers to pain management, psychological support, and quality-of-life comfort care available to both end-of-life patients and seriously ill patients in managed long-term care facilities or home care.
The authors of the new study note that “approximately 85% of MLTC users are over age 65 and are dealing with numerous chronic ailments and significant symptom burdens. About 20% of patients admitted to home health care, a key component of MLTC, die within 12 months, highlighting the urgent need to improve access to (palliative care) for this population’s complex needs.”
“The initial communication process to engage patients or their surrogate caregivers in palliative care remains underexplored,” the authors continue, “leaving a gap in understanding what makes it successful or unsuccessful.”
The authors concluded: “For geriatric nurses, integrating speech-recognition technology could transform how palliative care decision-making is initiated and supported. Older adults often face communication challenges related to cognitive decline, sensory impairment, or emotional distress, which may hinder clear expression of care preferences. Speech-based analytics can help clinicians recognize subtle vocal cues, such as hesitation, tone shifts, or reduced energy, that reflect uncertainty, discomfort, or readiness to engage in palliative care discussions. By interpreting these cues, nurses can adjust their communication strategies, clarify information, and foster trust more effectively.”
The study, “Leveraging Patient and their Surrogate Caregiver Communication with Clinicians to Predict Palliative Care Decisions: A Speech Processing Study,” was published in March, 2026 in Geriatric Nursing. Authors included Jiyoun Song, PhD, APRN, and Kathryn H. Bowles, PhD, RN.


Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

LDI Fellows’ Research Quantifies the Effects of High Health Care Costs for Consumers and Shines Light on Several Drivers of High U.S. Health Care Costs

Comment: Submitted to Centers for Medicare & Medicaid Services

A Licensure Model May Offer Safer Oversight as Clinical AI Grows More Complex, a Penn LDI Doctor Says

CF Foundation’s Landmark Drug Approvals With Vertex Inspired Patient Groups to Act Like Biotech Investors. But Only a Few Groups Have Made Big Bets, LDI Fellow Finds