Improving Care for Older Adults
Brief
Cost Impact of the Transitional Care Model for Hospitalized Cognitively Impaired Older Adults
Use of Advanced Practice Nurses can Lower Postacute Care Use and Costs

Mark V. Pauly, Karen B. Hirschman, Alexandra L. Hanlon, Liming Huang, Kathryn H. Bowles, Christine Bradway, Kathleen McCauley, & Mary D. Naylor
Journal of Comparative Effectiveness – published September 11, 2018
KEY FINDINGS
Using advanced practice nurses to support high risk patients and their families to transition from hospital to home can reduce postacute care use and costs. A study comparing three evidence-based care management interventions for a population of hospitalized older adults with cognitive impairment found that the Transitional Care Model, which relies on advanced practice nurses to deliver services from hospital to home, was associated with lower postacute care costs when compared to two “hospital only” interventions.
THE QUESTION
Hospitalized older adults with cognitive impairment and multiple chronic conditions are at higher risk for poor health outcomes, including high and costly use of postacute care services and hospital readmissions. In 2016, the average annual per-person payment for postacute care for Medicare beneficiaries with Alzheimer’s and other dementias was 11.5-times greater than older adults without dementia. While evidence-based care management interventions for this population exist, their impact on postacute care use and costs, and on overall costs in the six months after hospital discharge, remains unknown.
To shed light on these cost impacts, Mary Naylor, Mark Pauly, and colleagues compared three interventions of different intensity delivered to more than 200 hospitalized older adults with cognitive impairment. Three hospitals in one health system were randomized to one of these interventions:
- In Augmented Standard Care (“ASC,” lowest dose), trained research assistants screened patients for dementia on hospital admission and communicated positive findings to the medical/surgical team.
- In Resource Nurse Care (“RNC,” medium dose), trained registered nurses who demonstrated competency on web-based modules on dementia and delirium were designated as resource nurses for the hospital, and cared for participants or trained other nurses to do so.
- In the Transitional Care Model (“TCM,” highest dose), trained advanced practice nurses delivered services from hospital to home, which included visiting the patient in the hospital, meeting with the medical/ surgical care team daily, and following the patient to the next site of care, among other activities.
THE FINDINGS
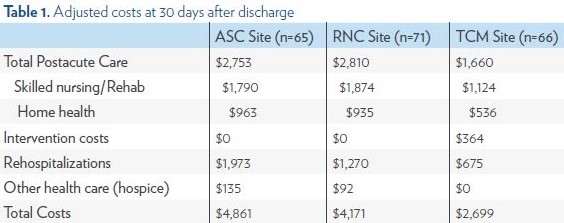
At 30 days after discharge, patients in the TCM site had significantly lower average postacute care (skilled nursing and home health) costs ($1,660, not including the additional costs of TCM) than patients in the RNC site ($2,810) and ASC site ($2,753). The TCM intervention costs averaged $364, including the time spent on visits, calls, travel, and documentation. At 30 days, patients in the TCM site had lower total costs ($2,699) than patients in the RNC site ($4,171) and the ASC site ($4,861), though these differences were only marginally statistically significant.
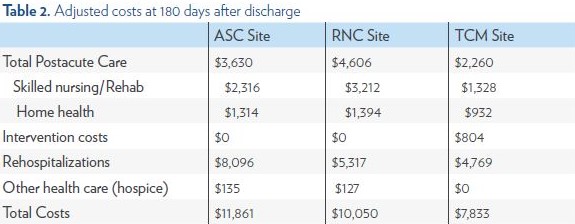
The findings were similar when average costs were calculated at 180 days after discharge, where the TCM group had lower postacute care costs ($2,260) than the RNC group ($4,606) and the ASC group ($3,630). TCM services, which extended for an average of two months beyond hospital discharge, cost an average of $804 at 180 days. The TCM group’s total average costs at this endpoint in the study were $7,833, compared to $10,050 in the RNC group and $11,861 in the ASC group.
The breakdown of costs at 30 and 180 days, by type of service, appears in Tables 1 and 2.
THE IMPLICATIONS
Use of specially trained nurses who can provide continuity of care between hospital and home can significantly reduce postacute care use and costs for high risk patients with cognitive impairment. TCM not only reduced the amount of postacute care services needed, such as home health visits or skilled nursing facility (SNF) stays, but also affected total costs of care after hospital discharge. The impact on SNF use – the single largest contributor to postacute care costs – was particularly significant: costs among the TCM group were about $1,000-$2,000 lower than the RNC and ASC groups 180 days after discharge. Additionally, reduced rehospitalization costs among individuals in the TCM group more than covered additional expenses associated with TCM implementation.
TCM can lower patients’ use of postacute care services and reduce the burden on caregivers. Future studies should examine the specific processes that bring about these lower costs in TCM or similar models, or ways to reduce TCM implementation costs without affecting the standard of care.
THE STUDY
This study compared postacute care and rehospitalization costs for hospitalized older adults with cognitive impairment who received one of three care management interventions. It occurred across three sites within the same urban academic medical system. Each site was randomly assigned to one of the three interventions (ASC, RNC, or TCM) and participants received the intervention at the site at which they received care. Statistical methods were used to adjust for potential selection bias since randomization of patients was not possible. The authors then compared postacute care and rehospitalization costs for participants in each intervention group at 30 days and 180 days after hospital discharge.
ABOUT THE AUTHORS
Mark V. Pauly, PhD is Bendheim Professor in the Department of Health Care Management, Professor of Health Care Management, and Business and Public Policy at The Wharton School and Professor of Economics in the School of Arts and Sciences at the University of Pennsylvania. He is one of the nation’s leading health economists. Most recently, he has examined the topics of national health care reform, the individual insurance market, the effects of poor health on worker productivity, and the market for voluntary health insurance in developing countries. He is currently studying how insurance affects the rate of growth of medical spending.

Mary D. Naylor, PhD, RN, FAAN is Marian S. Ware Professor and Director, NewCourtland Center for Transitions and Health, at the University of Pennsylvania School of Nursing. Over two decades she has designed, tested, implemented, and translated a model of transitional care to improve outcomes for older adults and their family caregivers. More than a decade of rigorous research has demonstrated the effectiveness of Dr. Naylor’s Transitional Care Model (TCM) using advanced practice nurse-led, team-based care management innovation. She has led the translation of her findings into wide adoption and has been a leader in building the evidence linking nursing to quality of care.