Brief
A National Comparison of Operative Outcomes of New and Experienced Surgeons
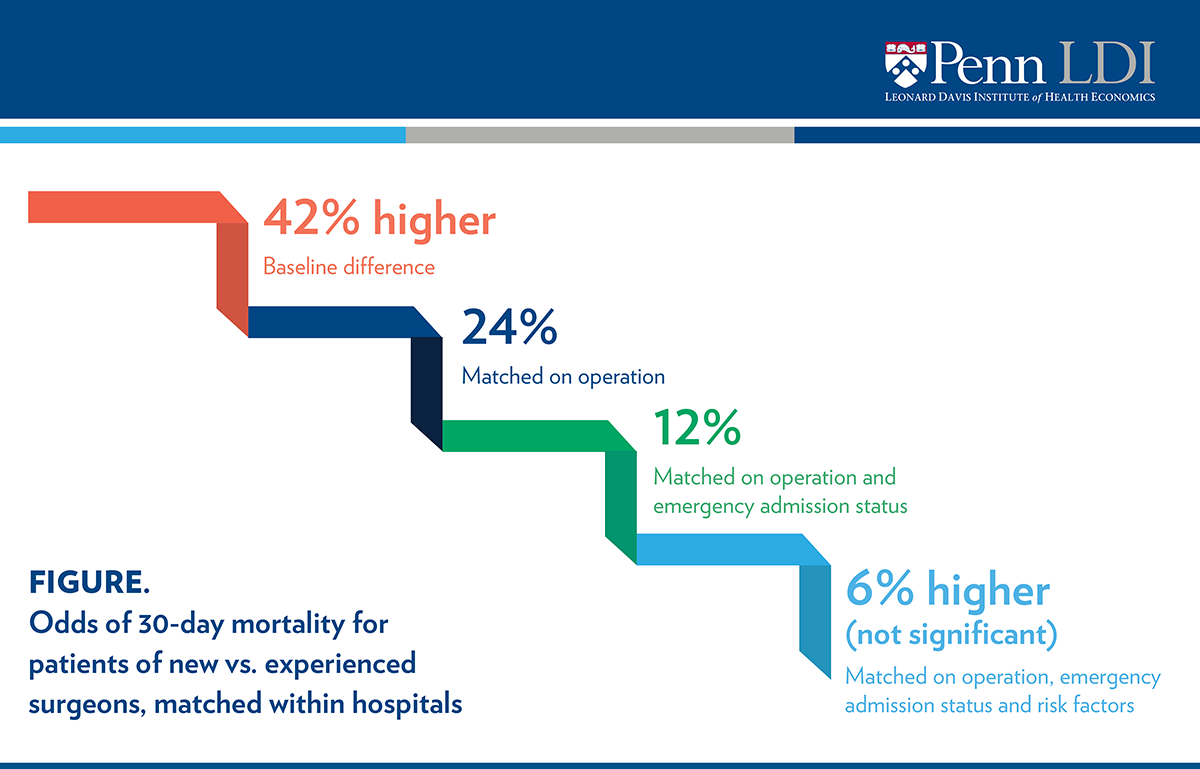
Case-mix, not physician experience, accounts for most differences in outcomes
Annals of Surgery – published online June 7, 2019

Key Findings
In this national study, Medicare beneficiaries treated by new surgeons had poorer outcomes than those treated by experienced ones in the same hospitals. However, the type of operation and the patient’s emergency status – rather than physician inexperience – explains nearly all poorer outcomes. Higher-risk cases are disproportionately treated by new surgeons.
The Question
While prior studies suggest that patients of new surgeons fare worse than those of experienced surgeons, it is unclear whether outcomes differ due to surgeon experience level or the context in which care is delivered. This study compares outcomes among fee-for-service Medicare beneficiaries receiving care from new and experienced surgeons at the same hospitals, taking into account operation type, emergency admission status, and patient risk factors, including comorbidities.
The authors investigated differences in 30-day mortality, as well as other clinical and utilization outcomes, among beneficiaries who underwent orthopedic or general surgery between 2009 and 2013. Surgeons were considered “new” within the first three years of practice, and “experienced” if they had at least 10 years of practice experience.
The Findings
More than 10,000 surgeons working in over 1,200 hospitals were includedin the study. After pairing new and experienced surgeons working at the same hospitals, the researchers compared 1,820 surgeons in each group. New surgeons had an average of 1.6 years of experience at the time of the operation, while experienced surgeons had an average of 21.3 years of experience.
Patients treated by new and experienced surgeons differed in meaningful ways. Compared to patients of experienced surgeons, patients of new surgeons at the same hospital were more likely to have presented at the emergency department (53.9% vs. 25.8%) and to be age 85 or older (25.8% vs. 16.3%). The type of operation differed as well: for example, total knee replacement comprised 16.8% of operations for new surgeons, compared to 47.5% for experienced surgeons. Not surprisingly, patients of new surgeons, upon admission, had a higher probability of 30-day mortality than patients of experienced surgeons.
After matching these surgeons by the year of the operation (baseline), patients of new surgeons had 42% higher odds of 30-day mortality than patients of their more experienced colleagues (6.2% vs. 4.5%). As shown in the Figure, matching by the type of operation reduced the difference in odds from 42% to 24%; further matching by emergency status of the patient reduced it to 12%. Further matching by patient risk factors and comorbidities reduced the difference to insignificant levels. Thus, operation type and emergency department admission status – not surgeon experience level – explain these differences in the odds of 30-day mortality rates.
The authors examined a number of other clinical outcomes, such as failure-to-rescue (death after developing a complication) and 30-day readmission and death, and found similar patterns. They also looked at process and utilization outcomes, including prolonged length of stay, anesthesia time, and resource use. They found similar, though more nuanced, patterns, with slight differences in some outcomes remaining after matching on different factors. For example, patients of new surgeons were slightly more likely to experience prolonged length of stay and require a longer anesthesia time (155.4 vs. 137.6 minutes) than patients of experienced patients, even when matched. Thirty-day resource costs for patients of new surgeons were $2,466 higher than experienced surgeons’ patients without matching, a difference that was halved ($1,257) after matching on the factors included in the study.
The Implications
This is the first national study of surgical outcomes for a comprehensive set of procedures performed by new and experienced surgeons. It reveals that poorer outcomes associated with new surgeons can mostly be explained by differences in their operative and case mix. Newer surgeons are typically treating older, sicker patients who are admitted on an emergency basis.
This study has important implications for both surgical education and practice. The matching methods may be useful in developing a robust audit and feedback system to assess the performance of surgical training programs, as graduate medical education programs move to an outcomes-based system of accreditation.
Even more importantly, it points to potential ways to minimize or eliminate outcome differences. Because new surgeons perform riskier operations, they might benefit from more attention from experienced surgeons prior to and during the operation in terms of operative judgment and technique. Because new surgeons operate on more complex patients, they might also benefit from guidelines that encourage them to discuss high-risk cases with an experienced colleague.
As the US faces an anticipated shortage of thousands of surgeons by 2030, the country will increasingly need to rely on new surgeons for care. Strategies to enhance support for new surgeons are needed as they transition to practice.
The Study
The authors first identified over 760,00 fee-for-service Medicare beneficiaries aged 65.5 or older who underwent orthopedic or general surgery from 2009 to 2013. Surgeons were considered “new” if they were within their first three years of independent practice. Those with ten or more years of independent practice were considered “experienced.”
New and experienced surgeons in the same hospital were paired for comparison. In total, 1,820 surgeons were identified in each group, and 10 randomly sampled patients of new surgeons were compared to four sets of patients of experienced surgeons. Each set of experienced surgeons’ patients was matched to patients of new surgeons by a characteristic that may have contributed to differences in patient outcomes, holding constant the matched characteristics from previous sets. The “baseline” set of patients was matched on year of operation, for example, while the fourth set of patients was matched on year of operation, type of operation, emergency department admission status and patient-level risk factors.
Lead Author

Rachel R. Kelz, MD, MSCE, MBA, FACS is a Professor of Surgery at the Perelman School of Medicine at the University of Pennsylvania. She is an Endocrine Surgeon and cares for patients at the Hospital of the University of Pennsylvania. Dr. Kelz serves as the Vice Chair of Clinical Research within the Department of Surgery. Dr. Kelz is recognized as a leader in surgical education and was awarded the Lindback Foundation award for distinguished teaching by the Provost of the University of Pennsylvania. She serves as the Surgeon Champion for the National Surgical Quality Improvement Program at Penn. Her work in outcomes and education has recently merged, and she is focusing on innovative approaches to combine administrative data with chart abstraction to identify opportunities to improve surgical education and performance.
All phases of this study were supported by National Institute on Aging/National Institutes of Health grant R01 AG049757. NIA/NIH had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript to submit for publication.