
Medicare’s Hidden Fix for High Drug Costs
Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print
Health Care Access & Coverage
Blog Post
There is broad agreement that there is plenty of wasteful and low-value care in our health care system. But there’s less agreement about how to identify it and even less agreement about what to do about it. Health insurers have taken different approaches to this problem. Some insurers have adopted prior authorization, a managed care tool that requires physicians to obtain insurer approval before performing particular services. The different approaches to prior authorization are made apparent in a new study in JAMA Health Forum by Aaron Schwartz and colleagues, in which they apply the typical coverage rules of a large Medicare Advantage plan to fee-for-service Medicare, which lacks prior authorization. They find that about 25% of all spending on Medicare Part B outpatient services would be subject to prior authorization if the private plan rules applied.
The authors analyzed fee-for-service Medicare claims from 2017 for beneficiaries in Medicare Part B. More than 40% of the 6.5 million beneficiaries received at least one service per year that would have been subject to prior authorization under Medicare Advantage plan rules. On average, there were 2.2 such services per beneficiary per year, with highest rates of preauthorization required for services delivered by radiation oncologists (97%), cardiologists (93%), and radiologists (91%), and lowest rates among pathologists (2%) and psychiatrists (4%).
The services subject to prior authorization accounted for $1,661 in spending per beneficiary per year (25% of total annual Part B spending). Part B drugs (typically, injectable drugs) constituted 58% of the associated spending, mostly accounted for by hematology/oncology drugs, as shown in Figure 1. Radiology was the largest source of non-drug spending (16%), followed by musculoskeletal services (9%).
To be clear, if Medicare adopted prior authorization policies like private insurers, we don’t know exactly how much money it would save or how many unnecessary services would be avoided. Although the authors described how often prior authorization requests tend to be denied, it is not known how often the rules deter physicians from applying for prior authorization. But it is clear that private insurers in Medicare have a vastly different approach to coverage policy than traditional Medicare. When it comes to the use of wasteful health care services, traditional Medicare has limited tools to confirm that medical care is necessary, and policymakers may face political pressures to avoid denials of coverage. Private insurers have more managed care tools at their disposal, like prior authorization, though physicians can find these administratively burdensome. While we can’t say which approach is the better one, these findings suggest that private managed care plans have decided that a significant percentage of Medicare spending may be worth reviewing ahead of time to confirm its medical necessity.
The study, Measuring the Scope of Prior Authorization Policies: Applying Private Insurer Rules to Medicare Part B, was published in JAMA Health Forum in May 2021. Authors include Aaron L. Schwartz, Troyen A. Brennan, Dorothea J. Verbrugge, and Joseph P. Newhouse.

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools

A 2024 Study Showing How Even Small Copays Reduce PrEP Use Fueled Media, Legal, and Advocacy Efforts As Courts Weighed a Case Threatening No-Cost Preventive Care for Millions
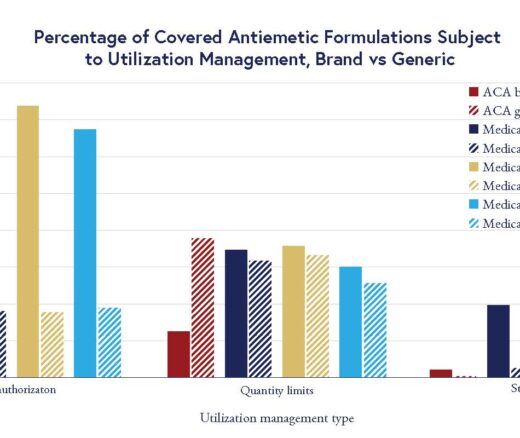
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use