Health Care Access & Coverage
Blog Post
Chart of the Day: Adverse Tiering for HIV/AIDS Patients
It’s called “adverse tiering” and it’s a benefit strategy designed to dissuade patients with expensive chronic conditions from enrolling in marketplace plans. The ACA prohibited plans from refusing to cover patients with pre-existing conditions and from charging them higher premiums. To avoid high-cost patients, some plans have structured their formularies to require substantial cost sharing for drugs in a certain class, particularly for expensive conditions such as HIV/AIDS.
Adverse tiering received no attention in the recently failed Congressional efforts to repeal-and-replace the ACA, but pre-existing conditions and Medicaid were two of the hottest points of contention. In a Health Affairs blog post, Justin Puckett and LDI Senior Fellow Jalpa Doshi point out that Congress has ignored a subtle connection between Medicaid expansion and coverage of pre-existing conditions, one that could promote adverse tiering if Medicaid expansion is phased out or eliminated.
The idea is that in Medicaid expansion states, many low-income, chronically ill patients were covered by Medicaid instead of private plans, minimizing the likelihood that plans would discriminate through adverse tiering. To demonstrate this effect, Puckett and Doshi examined how adverse tiering (defined as percentage of marketplace plans placing all multi-class combination products used to treat HIV on a specialty tier) varies for patients with HIV/AIDS between expansion and non-expansion states. The authors also compared these practices to the state of Louisiana, which expanded Medicaid in 2016-2017.
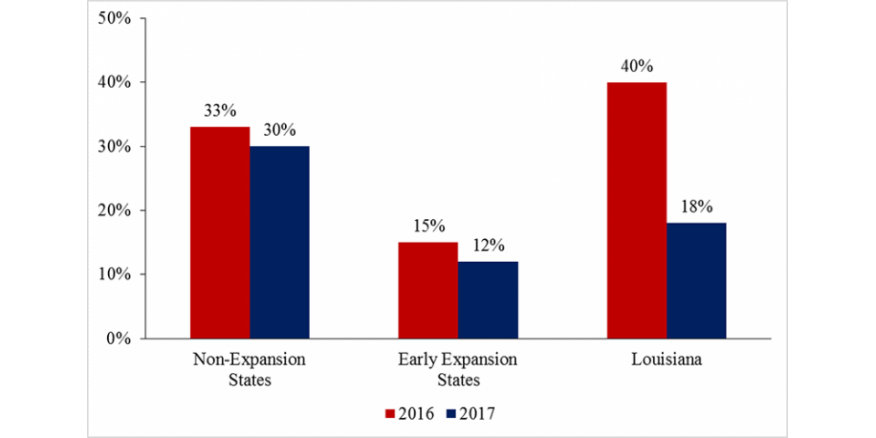
Their analysis revealed that adverse tiering is a much greater problem in states that have not expanded Medicaid. Further, Medicaid expansion in Louisiana seemed to have reduced the prevalence of adverse tiering. The authors note the policy implications of their work:
Although ideological opposition to the Medicaid expansion makes its future uncertain, policymakers should be cognizant of the unintended consequences of modifying the expansion. They should also be aware that insurers may expand their use of adverse tiering in order to circumvent protections for individuals with preexisting conditions, leaving sicker, low-income patients with ineffectual coverage and no viable alternative. Any serious replacement proposal that seeks to maintain protections for these patients while rolling back the Medicaid expansion must grapple with the fact that guaranteed issue does not always mean guaranteed access.