Health Care Access & Coverage
Blog Post
Delayed Emergencies in COVID
Patterns of Deferred Care
COVID-19 changed every aspect of our lives, from shopping for groceries to visiting doctors. Early public health messages encouraged people who thought they could put off emergency care to avoid the emergency department (ED), to save capacity for an anticipated surge of COVID cases. Our new study confirms earlier findings from the Centers for Disease Control and Prevention (CDC) showing quite how often this occurred. It also gives us new insights into who stayed home and what kind of care they deferred.
We studied EDs in Louisiana, one of the earliest and hardest-hit areas of the country. A partnership between the Leonard Davis Institute (led by LDI Senior Fellow Guy David, PhD), Blue Cross and Blue Shield of Louisiana (led by Somesh Nigam, PhD), and Gunnarsson Consulting used claims data to assess patterns across a broad swath of EDs. Not surprisingly, we found that utilization of EDs declined dramatically in a short period of time. But the magnitude and specific patterns were unexpected.
As shown in Figure 1, we found that ED visits for non-respiratory complaints declined by 39% at the beginning of the pandemic, using a differences-in-differences approach (that is, comparing the change from January 1, 2020–March 7, 2020 to March 8, 2020–May 16, 2020 to equivalent dates in 2019).
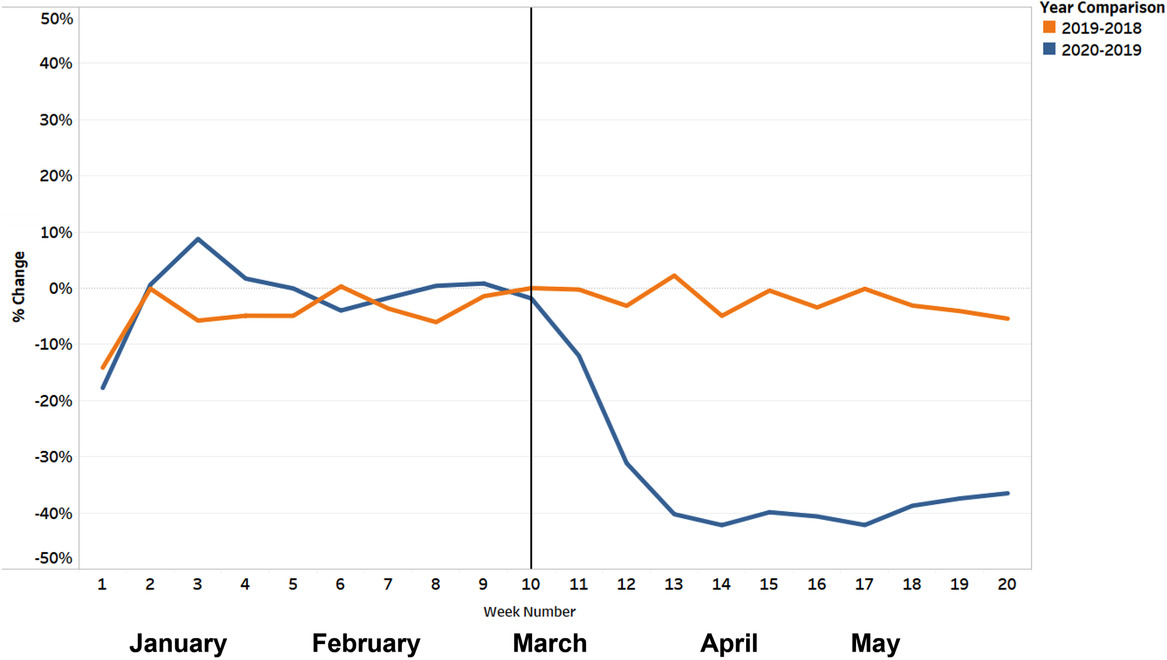
Our findings are remarkably consistent with the CDC, which found ED visits declined by 42% from March 29-April 25, 2020, when compared to similar dates in 2019. The CDC data provides a national scope but has some limitations, including a shift in the hospitals included over time.
Within those large overall declines, our study sheds light on who stayed home and what kinds of care they deferred.
Some of the patterns reflect understandable responses by the public. Respiratory complaints surged during the pandemic, likely reflecting COVID’s rapid emergence. Influenza visits were minimal compared to a typical flu season, likely driven by masking and distancing. Across all non-respiratory conditions, patients residing in areas of high COVID-19 prevalence were 22.7% less likely to visit the ED.
Using a standard algorithm for categorizing ED visits, we found that “deferrable” visits dropped more than 50%. Many of these visits could likely be seen in other, lower-cost, settings or pulled to other settings through more robust primary care. For instance, ear conditions, muscle strains, and urinary tract infections all declined and are all generally mild conditions potentially amenable to care in other settings, improving the value proposition.
Other patterns of who stayed home are more worrying. “Non-deferrable” visits still dropped more than 30%. Patients at high risk for COVID complications, such as those with asthma, diabetes, and end-stage renal disease, reduced their ED visits more than those without those risk factors. Patients over 65, even the oldest old (85+) were less likely to seek ED care, despite their higher risk of complications from avoiding care. These groups were at greater risk of COVID complications, so in the early days of the pandemic when it was less clear that masking and other precautions made hospitals safer than restaurants and other public settings, this was logical. Nevertheless it may not have been safe for patients.
In our study of ED claims, we can’t know whether many of these patients sought or received alternative forms of care. Did the decline in ED visits reflect increased remote access to patients’ usual providers through telemedicine? If so, this represents a rapid change that might endure beyond the pandemic, potentially saving costs. Or did many patients delay seeking medical attention entirely, even for potentially life-threatening conditions?
National mortality patterns give us cause for concern. Multiple studies have found “excess mortality” during the pandemic beyond COVID-related deaths; overall, all-cause deaths are higher right now than even the COVID-specific numbers would suggest. The New York Times recently estimated that 494,000 more Americans died since March than they would have in a normal year. One potential reason: deferred ED care for serious conditions. Studies point to alarming decreases in non-elective cardiac catheterizations for myocardial infarction and in emergency stroke alerts at several large U.S. academic hospitals – severe conditions amenable to medical and procedural intervention.
The emergency department has long served as the safety net for the U.S. health care system across a broad spectrum of disease severity, from earaches to heart attacks. COVID-19 is a capacity-sensitive disease. Therefore, initial messaging to avoid the ED may have saved lives. However, that messaging seems also to have deterred patients with potentially life-threatening conditions from presenting to EDs. Experts should plan an early transition in future pandemic messaging from discouraging ED visits to encouraging normal care. Throughout the pandemic they should keep messaging nuanced to focus on moving lower-acuity ED visits to telemedicine and other care settings while emphasizing the importance of seeking ED care for more severe symptoms.
The study, Delayed Emergencies: The Composition and Magnitude of Non-Respiratory Emergency Department Visits During the COVID-19 Pandemic, was published in Journal of the American College of Emergency Physicians Open in February 2021. Authors include Ari B. Friedman, Deidre Barfield, Guy David, Thomas Diller, Candace Gunnarson, Miao Liu, Benjamin V. Vicidomina, Ruthann Zhang, Yuan Zhang, and Somesh C. Nigam.