Blog Post
The Evolving Role of Academia During the COVID-19 Pandemic
Lessons from Colorado
Colorado’s response to the COVID-19 pandemic has been informed by an evolving partnership between academia and public health practitioners that can serve as a model for other states. As a core member of the COVID-19 Modeling Group—organized as the pandemic reached Colorado—my work is focused on informing hospital and local health department capacity to mitigate and suppress COVID-19. I also lead the development of a public-facing website to track indicators relevant to the pandemic.
My engagement began on March 17 when I received an e-mail from the Dean of the Colorado School of Public Health asking: “Do you have the Census data in hand? May want it for modeling the epidemic.” At that point, Colorado had identified 30 cases of COVID-19 and Governor Jared Polis had issued an executive order to suspend all downhill skiing operations. In the weeks to come, the numbers would grow exponentially.
The Dean was convening the multidisciplinary COVID-19 Modeling Group to work closely with the Governor, state health department, and local stakeholders. The state’s early response to the pandemic focused on ensuring that hospitals had sufficient surge capacity to serve the potentially overwhelming number of patients with COVID-19 complications. Accordingly, the Modeling Group’s priority was to develop an epidemic model using Colorado data, which has since become a foundation for the state’s evidence-based policies.
Understanding Local Health Department Capacity for Contact Tracing
By mid-April, understanding contact tracing capacity emerged as another priority. Case identification and contact tracing are critical components in a comprehensive approach to contain and eventually suppress the COVID-19 pandemic, especially as businesses, public schools, and universities try to reopen.
Colorado needed to assess the baseline capacity of its 53 local health departments to conduct COVID-19 contact tracing activities. To facilitate a data-informed approach to workforce planning and allocation, the Colorado School of Public Health collaborated with the Colorado Association of Local Public Health Officials, the Colorado Department of Public Health & Environment and members of the Colorado Public Health Workforce Collaborative to develop and administer the Colorado Local Public Health Agency Contact Tracing Workforce and Technical Capacity Survey. There have also been other efforts to understand contact tracing capacity that have mostly found gaps similar to those identified through the survey.
Gaps in Contact Tracing and Urban-Rural Differences
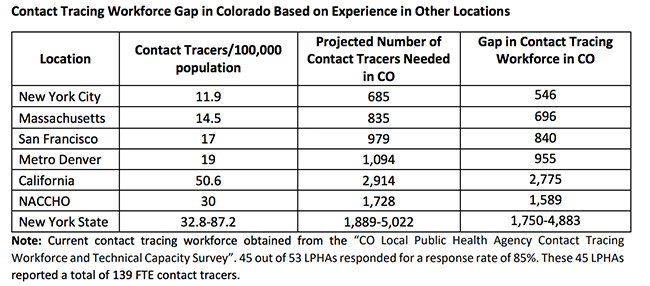
Forty-five local public health departments reported a total of 115 full-time equivalent (FTE) contact tracers. The study identified large gaps in the state’s public health capacity to implement a comprehensive contact tracing program. Based on experience in different U.S. jurisdictions and expert projections given Colorado’s population size, the gap in the contact tracing workforce in the state was between 570 and 4,907 (Figure 1). The gap was larger for rural and frontier counties, but more than 90% of the public health departments needed more contact tracers than they had.
Many of the existing contact tracers came from temporary redeployments of personnel from health departments or other government agencies. These temporary solutions were critical in the early local response to the pandemic; however, the consensus was that in the long term, health departments would need additional funding to hire and train contact tracing personnel.
Prioritization of Contact Tracing Efforts
Limited capacity meant that local health departments had to prioritize segments of the population for contact tracing. Older adults, residents with diseases and conditions associated with severe COVID-19 disease, and essential workers were a priority for contact tracing efforts. Only 42% of health departments focused their efforts on homeless people, citing the complexity of obtaining information from that population.
Technological Infrastructure and Capacity
In the absence of a centralized electronic state platform to collect contact tracing data, health departments developed their own solutions, resulting in a poorly-coordinated and fragmented approach. These “home-grown” electronic platforms ranged from manually managed Excel spreadsheets and paper-based data entry to Google applications. Here is a problem needing a rapid solution and one that reflects long-standing inattention to public health infrastructure.
It’s Not Just About the Number of Contact Tracers…
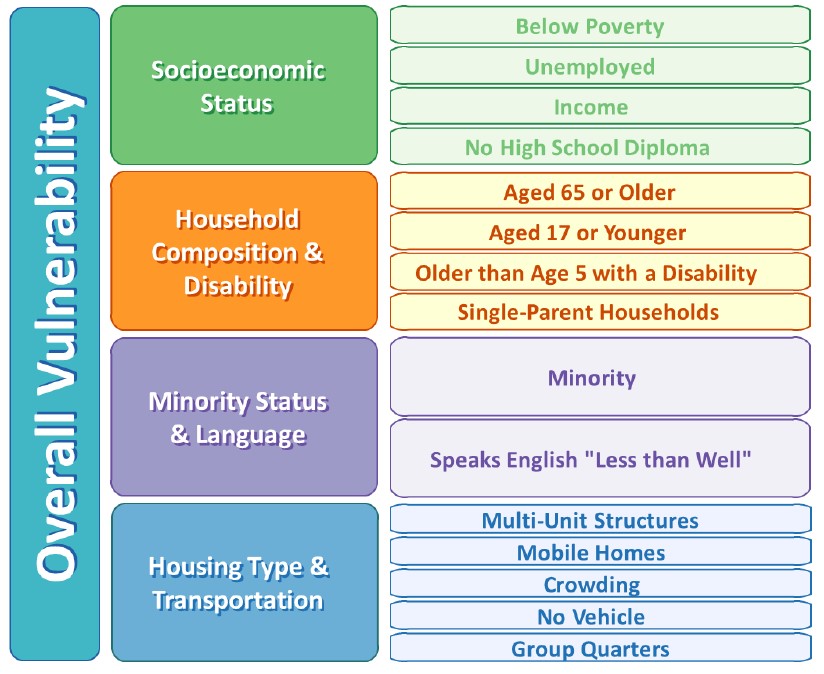
The study group recommended that the state integrate demographic and socioeconomic characteristics into its planning for a more equitable workforce allocation. We proposed using the Centers for Disease Control & Prevention (CDC) Social Vulnerability Index (SVI) (Figure 2) to help anticipate the underlying needs of a community and make workforce allocations accordingly. For instance, the ability to quarantine for 14 days is critical to effective contact tracing. In counties with high levels of vulnerability, residents may need to be connected to community resources to successfully complete the voluntary quarantine. In this case, the “Resource Coordinators” may be central to the success of contact tracing efforts and counties may need to prioritize hiring these workers.
Policy Implications
As the first deliverable of the emerging Colorado Public Health Workforce Collaborative, the report recommended ways to augment contact tracing capacity. It informed the allocation of new state and federal dollars to aid local health departments in their COVID-19 response efforts. It also provided the first snapshot of the state’s contact tracing capacity, and a baseline for monitoring Colorado’s progress in filling the identified gaps.
Since the June report, state and local health departments have hired and trained hundreds of contact tracers, including volunteers from an AmeriCorps initiative. The state is currently piloting a centralized contact tracing system to support systematic and standardized data collection.
As the pandemic evolves, so has the role of this academic-practitioner partnership. From its initial focus on modeling, the Collaborative’s work has expanded to examine local health department contact tracing capacity, the impact on mobility patterns as social distancing is relaxed, the impact on the supply and demand side of local economies, and the creation of a website to disseminate its work to a broader audience of stakeholders. This expanded portfolio reflects the needs of our local partners and illustrates the central role academia can play in suppressing the COVID-19 pandemic. One elected official summarized this partnership as follows:
“I think it’s [epidemic model, data and website] very helpful from the standpoint of…as you speak with us [elected officials] and hear what we have to say, it sounds like it may help refine the output and that output will become more relevant to our needs…and…it’s very helpful for us because those of us [elected officials]…we are swimming in the dark, but yet we’re responsible for making and enforcing policy…and…all of this helps.”
Tatiane Santos, PhD, MPH is an LDI Associate Fellow, a Postdoctoral Fellow at the Wharton School, and a core member of the Colorado School of Public Health COVID-19 Modeling Team.