Health Equity
Blog Post
How Health Systems Can Help Address Language Barriers to Achieve Digital Health Equity
From the CHOP PolicyLab Blog
[Cross-posted from CHOP PolicyLab]
The parents of a 7-year-old girl call their clinic with concerns about the health of their daughter. A telehealth visit is scheduled. On the day of the appointment, her parents, who speak and read a language other than English, are unable to navigate the patient portal account to join the virtual visit. She subsequently misses the appointment and experiences months with declining health and school performance that could have been avoided with early diagnosis and treatment.
Telemedicine provides incredible opportunities for patient access and engagement that could mitigate limitations often experienced by vulnerable families. However, like we see in the case above, those benefits may not be enjoyed equally by all.
Telemedicine as a Solution to Help Families Access Care
Early in the COVID-19 pandemic, under state-mandated stay-at-home orders, families suddenly faced new barriers to visiting their health care providers, including risk of COVID-19 exposure, decreased public transportation and limited in-person appointment availability. At Children’s Hospital of Philadelphia (CHOP), outpatient visits dropped to almost 20% of pre-pandemic seasonal volume. Telemedicine—the delivery of health care via remote technologies—became a vital link to health care, at one point accounting for 50% of outpatient visits. Beyond safely accessing care from home during a pandemic, telemedicine visits provides significant benefits for families by decreasing the loss of caregiver workdays, allowing for behavioral assessments in home environments and overcoming transportation barriers.
The Benefits of Telemedicine Have Not Been Realized Equitably
Unfortunately, increasing evidence has emerged that the advantages of telemedicine have not been realized equitably, especially by historically marginalized populations, racial and ethnic minority groups, refugee and migrant populations, patients with Emerging English Proficiency (EEP), patients in rural areas, and individuals with disabilities.
Among these groups at risk of worsening access to health care, the challenges faced by patients and families with EEP provide insights into important digital equity considerations. Patients and families with EEP live at the intersection of many social, economic and cultural challenges that create a digital divide, defined as the technology, internet, design usability, and empowerment access gaps between marginalized populations and others.
These obstacles are further exacerbated by health care systems and technologies that are designed with English speakers in mind.
This has a large and important impact. The number of U.S. residents who self-report as having Limited English Proficiency, a term used by the U.S. Census Bureau to describe those who speak English less than “very well,” has increased substantially in recent decades. These individuals now represent 9% of the U.S. population, or more than 25 million individuals. In Philadelphia, 23.9% of citizens speak a non-English language, which is higher than the national average of 21.9%. Notably, 16% of U.S. children live with at least one parent with LEP, including 43% of Latino and Asian American children.
As one family told us, “language is everything.” The ability to access telemedicine may worsen health care disparities, but that doesn’t have to be the case.
Opportunities for Health Systems to Close the Gaps in Telemedicine Care
To date, policy recommendations to improve telemedicine equity include increasing access to digital technology, digital literacy training and broadband internet.
Health care institutions must integrate equity into telemedicine programs from the start by considering where disparities could be exacerbated by systems-generated barriers, identifying solutions to overcome these barriers and auditing equity metrics throughout the program’s existence.
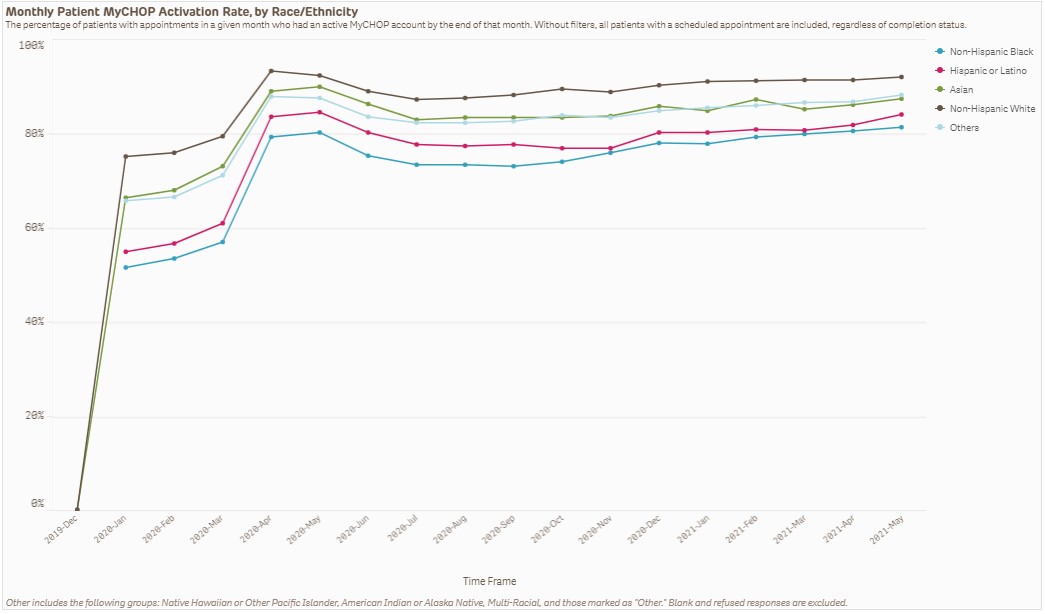
For example, patient portal accounts at CHOP provide an important access route to video visits with an interpreter—when a patient activates the portal account, it means they were able to successfully navigate the portal and can schedule and participate in video visits. As multilingual video visits increased at CHOP during the pandemic, our registration and clinic staff, as well as community health workers, led efforts that resulted in a 35% increase in patient portal activation rates for Spanish-speaking patients between January 2020-2021. Though the gap in portal activation was narrowed by 17% between English- and Spanish-speaking patients, significant disparities persist as our English-speaking patient population has 33% more patients with activated portal accounts than our Spanish-speaking patient population.
Based on our experiences, the following guiding principles could be followed as health systems continue to improve access to telehealth services for all populations:
- Establish digital health equity as a strategic priority. Dedicate time and effort to guide innovative solutions, raise awareness of health equity concepts, share ongoing equity work across the institution and engage key stakeholder voices including patients, community health workers, language service teams, nurses, registration staff, clinicians and community-based organizations.
- Invest in innovative multilingual digital health technology. Ideally, equity starts with the initial contracting and purchasing of a telemedicine platform. Invest in platforms that support multilingual user interfaces, including non-Romance and right-to-left languages. Telemedicine navigation steps must be simple: application downloads and account creation should be easy, and the platform should be able to accommodate phone-based visits and sign language needs. Platforms should seamlessly integrate interpreters, including third party vendors and sign language interpreters.
- Allocate resources for multilingual digital health support. Establish helpdesks and texting capabilities for video visits to ensure families with EEP receive adequate information about platform activation and technology requirements. Prepare to support families across language, literacy and digital literacy differences.
- Integrate equity into data analytics. Improve the accurate and consistent collection of demographic data, including EEP status and language preferences. Consistently report and review equity-related quality measures in telemedicine program analyses, such as how many families with EEP were able to activate their portal account, log in, join a telemedicine visit and successfully complete a high-quality telemedicine visit with an interpreter.
- Incorporate multilingual patient experiences into user-centered design decisions. Establish systematic methods through which patients and caregivers with EEP have the opportunity to co-design, test, and critically review changes to patient-facing technology to ensure acceptability and accessibility, including simplifying interfaces and navigation steps.
Overall, health care systems must take more immediate action to mitigate health system-generated barriers to telemedicine access. Linguistically appropriate and accessible virtual care should be a priority, both now and after the COVID-19 pandemic subsides. By adopting these guiding principles and taking a proactive stance, pediatric institutions can ensure digital health innovations need not be retrofitted to achieve digital health equity. Ultimately, care that is inequitable is not quality care.