Blog Post
Improving Emergency Care for Self-Harm Patients
Look to nurse leadership
Every year, about 500,000 patients present to emergency departments (EDs) across the country for deliberate self-harm, making the ED an important setting for suicide prevention services. Despite the need, less than 50% of hospitals offer certain evidence-based safety planning and other self-harm management practices. In a series of studies, my colleagues and I assessed the availability of key mental health services to ED patients after an episode of deliberate self-harm, and sought to understand how ED Directors perceived quality of care in the presence (or absence) of these practices.
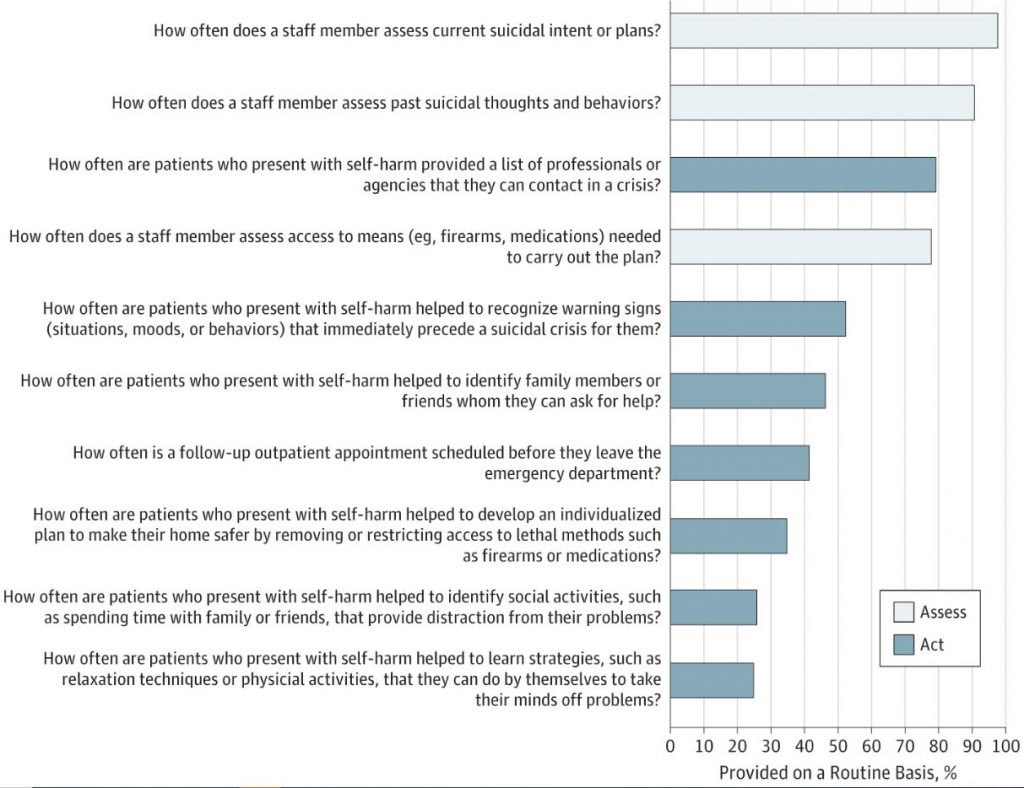
We surveyed ED Directors (mostly nurse managers) at more than 500 hospitals across the country to understand the frequency with which they implemented evidence-based, self-harm management processes. We also asked about mental health staffing levels, and their concerns about necessary resources.
In JAMA Psychiatry, our team (led by Steve Marcus, Jeff Bridge, and colleagues) found that while most hospitals routinely assess patients for self-harm, only 15.3% of hospitals regularly provide all recommended safety planning elements.
In our most recent article in the Journal of the American Psychiatric Nursing Association, we summarize nurse managers’ perceptions of the quality of care for these patients in their EDs. Teaching hospital status and higher levels of mental health staffing were associated with higher perceived quality of care. Nurse managers in EDs routinely using discharge and safety planning rated the quality of care nearly a full point higher (on a 5-point scale) than those not using these evidence-based practices regularly.
When it comes to improving hospital practice, buy-in from on-the-ground staff is necessary to implement change. Our results offer an optimistic message: ED nurse managers’ perceptions of the necessary practices to improve quality of care for deliberate self-harm patients are aligned with evidence-based recommendations. Understanding the need for these practices hopefully makes these nurse leaders more receptive to positive change.
ED nurse managers are well positioned to lead these efforts. Unfortunately, many hospitals lack dedicated mental health staff in their EDs, and hiring additional professionals may be cost prohibitive. For resource-constrained hospitals, educating current staff in evidence-based discharge and safety planning could help improve linkages with outpatient services and outcomes for this vulnerable population, without overburdening ED resources. Education tools on assessment and safety planning – accessible at little to no cost – could be used by clinical staff even at the smallest, most rural, or resource-strained hospitals. If properly provided, these practices can reduce the risk of repeated deliberate self-harm and future suicide attempts.