Blog Post
Inside the Black Box of Patient-Centered Medical Homes
Implementation is key to performance
The concept of a patient-centered medical home (PCMH) holds intuitive appeal, with its emphasis on coordination of care, improved patient-provider communication and patient engagement, use of health information technology, and expanded practice hours. However, evidence on its effects on utilization, quality, and costs has been mixed.

In two new papers, “The Economics of Patient-Centered Care” in the Journal of Health Economics and “The Impact of Patient-Centered Medical Homes on Medication Adherence” forthcoming in Health Economics, LDI Senior Fellow Guy David and coauthors give us one reason for the mixed results, namely, that the PCMH model is implemented differently across practices. In the first paper, David and coauthors Philip Saynisch and Aaron Smith-McLallen show how these differences drive variation in health care utilization and spending. In the second, David, Saynisch and Smith-McLallen, along with Spencer Luster and Ravi Chawla, explore the impact of variation in PCMH implementation on medication adherence.
In the Journal of Health Economics, David and colleagues use exceptionally detailed data to document specific PCMH capabilities in 104 practices that gained National Committee for Quality Assurance (NCQA) recognition as medical homes between 2008 and 2012. The dataset describes specific PCMH components in place, including scores based on 127 individual “factors” of implementation. They link these data with patient-level claims data on 152,093 HMO enrollees over six years (370,764 patient-years in total) covered by a large, private insurer in southeastern Pennsylvania. They track health care utilization and expenditures, before and after a practice transitions to a PCMH, through 2013.
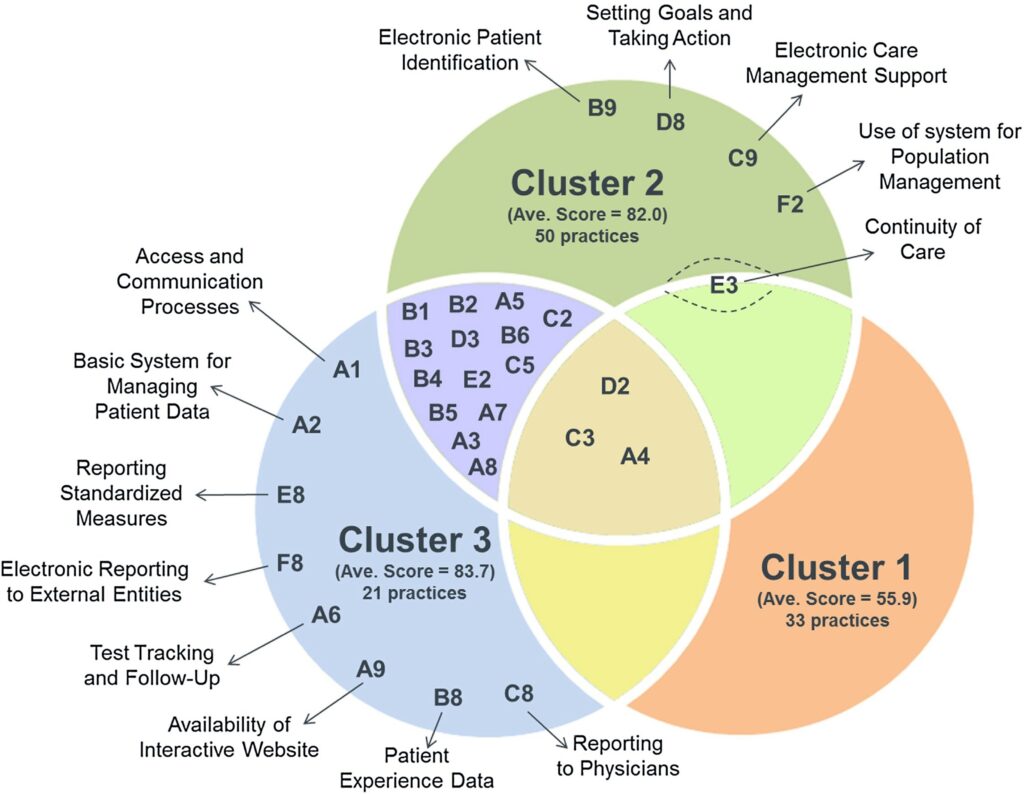
First, the authors grouped practices into one of three types using a hierarchical clustering approach:
► Cluster 1 – generally summarized as the “basic model,” which passes only minimum PCMH requirements;
► Cluster 2 – a “patient-facing” model emphasizing population health management; and
► Cluster 3 – a “physician-facing” model, a more technology-intensive approach emphasizing enhanced access, decision support, and data reporting.
The Venn diagram below illustrates this clustering, using the “points” each cluster received for each of 30 PCMH “elements.” If one cluster dominated the other two (in terms of implementation), the element label appears in only one circle; if two clusters dominated the third, the element label appears in the bullet-shaped area shared by the two clusters’ regions. The center area includes the elements for which no cluster had a clear advantage over the others:
For each cluster, the authors assessed the impact of implementing a PCMH on a variety of patient outcomes, including health care utilization (hospital admissions, primary care or specialist visits, and emergency department visits) and per-patient expenditures. They find that, when PCMH practices are assessed as one undifferentiated intervention, implementation has little impact on these outcomes. But when evaluating the outcomes for each cluster, a different picture emerges.
Practices in Clusters 2 and 3 have increased intensity of primary care utilization (both in terms of the likelihood of having any visit and the number of visits), consistent with greater adoption of new capabilities. Cluster 2 has more specialist visits and hospitalizations for chronically ill patients, consistent with outreach leading to greater intensity. Conversely, practices in Cluster 3 have an offsetting reduction in hospitalizations. Practices in Cluster 1, the most basic model, have reduced primary care utilization, without significant decreases in spending. This may be because Cluster 1 practices also have an increase in emergency department utilization, pointing to a possible substitution of lower-intensity primary care services for those provided in the ED.
Overall, these findings demonstrate that greater implementation is associated with improved performance – Clusters 2 and 3 have greater overall PCMH implementation scores, and both provide more primary care. At least in the case of Cluster 3, some evidence suggests that care is provided at lower cost and with fewer hospitalizations.
In the second study, forthcoming in Health Economics, David and colleagues used the same detailed implementation data from 134 primary care practices in southeastern Pennsylvania (the 104 practices in the study above, plus 30 additional pediatric clinics) to assess the medical home’s impact on medication adherence. To do so, the authors collaborated with NCQA to identify six components of the PCMH recognition guidelines that dealt particularly closely with medication adherence: organizing clinical data, use of system for population management, care management for important conditions, electronic prescription writing, and separate items for safety and efficacy under prescribing decision support. Practices were then categorized by how many of these capabilities they had adopted.
The figure below shows compares the number of elements adopted (on the x-axis) with the total overall performance on the PCMH recognition score (y-axis). This shows both the wide range of approaches practices took to implementing adherence-related PCMH capabilities, as well as demonstrating that a practice’s focus on boosting adherence wasn’t perfectly correlated with its overall PCMH score.
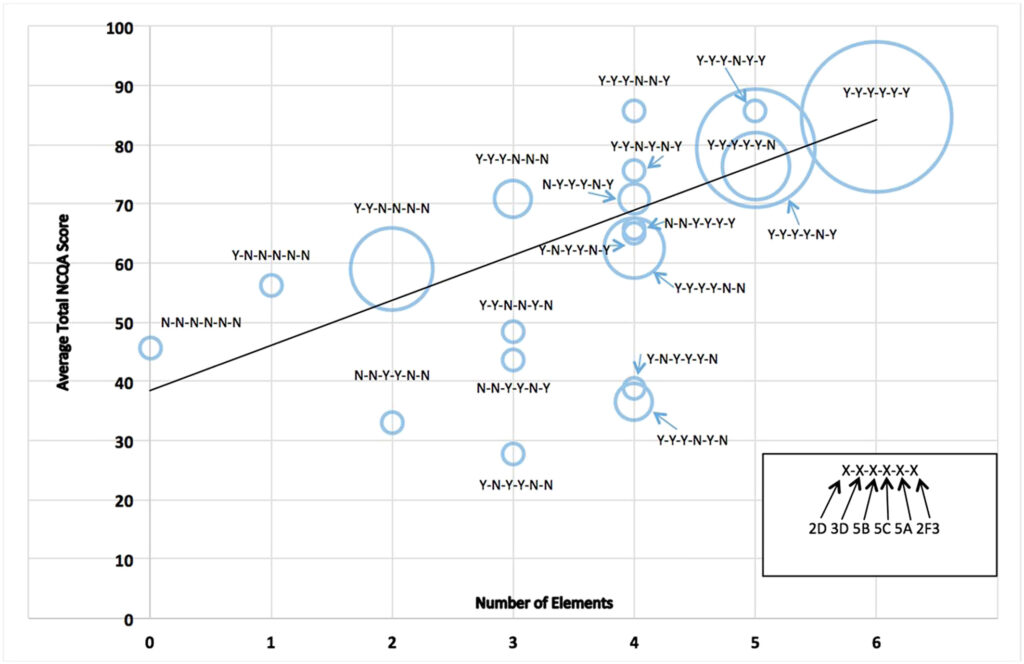
Source: David G, Saynisch P, Luster S, Smith‐McLallen A, Chawla R. The impact of patient‐centered medical homes on medication adherence?. Health Economics. 2018;1–16.
The authors find that adoption of the PCMH model results in a greater than 2 percentage point increase in overall adherence, as well as leading to improvements in adherence to specific medications like lipid control agents, beta blockers, anti-depressants and ACE inhibitors. This study also finds no effect in the practices that adopted 0 to 3 of the adherence-related capabilities, with the effect concentrated in those adopting 5 or 6. While 2.1 percentage points may seem like a small effect, this falls within the range of estimates for a much higher-powered policy lever aimed at improving adherence: reducing or eliminating copays for prescription medications.
These studies offer both potentially useful typologies of PCMH practices and viable strategies for evaluating the different ways that practices have implemented the PCMH model. The investigators are now conducting a much larger study of nearly 10,000 practices nationwide, repeating the clustering approach on a large enough group to validate the methods, assess the features that differentiate clusters in the national sample, and repeat the patient-level analyses on a larger and more geographically diverse population.