Health Care Access & Coverage | Substance Use Disorder
Blog Post
Medicaid Expansion and the Opioid Epidemic
New evidence that expansion reduces overdose mortality and increases treatment access
Despite little evidence, some commentators and policymakers have argued that Medicaid expansion has fueled the opioid epidemic by increasing access to prescription opioids. But a growing number of studies refute this theory, and instead suggest that Medicaid expansion reduces mortality from drug overdoses and increases access to drug treatment.
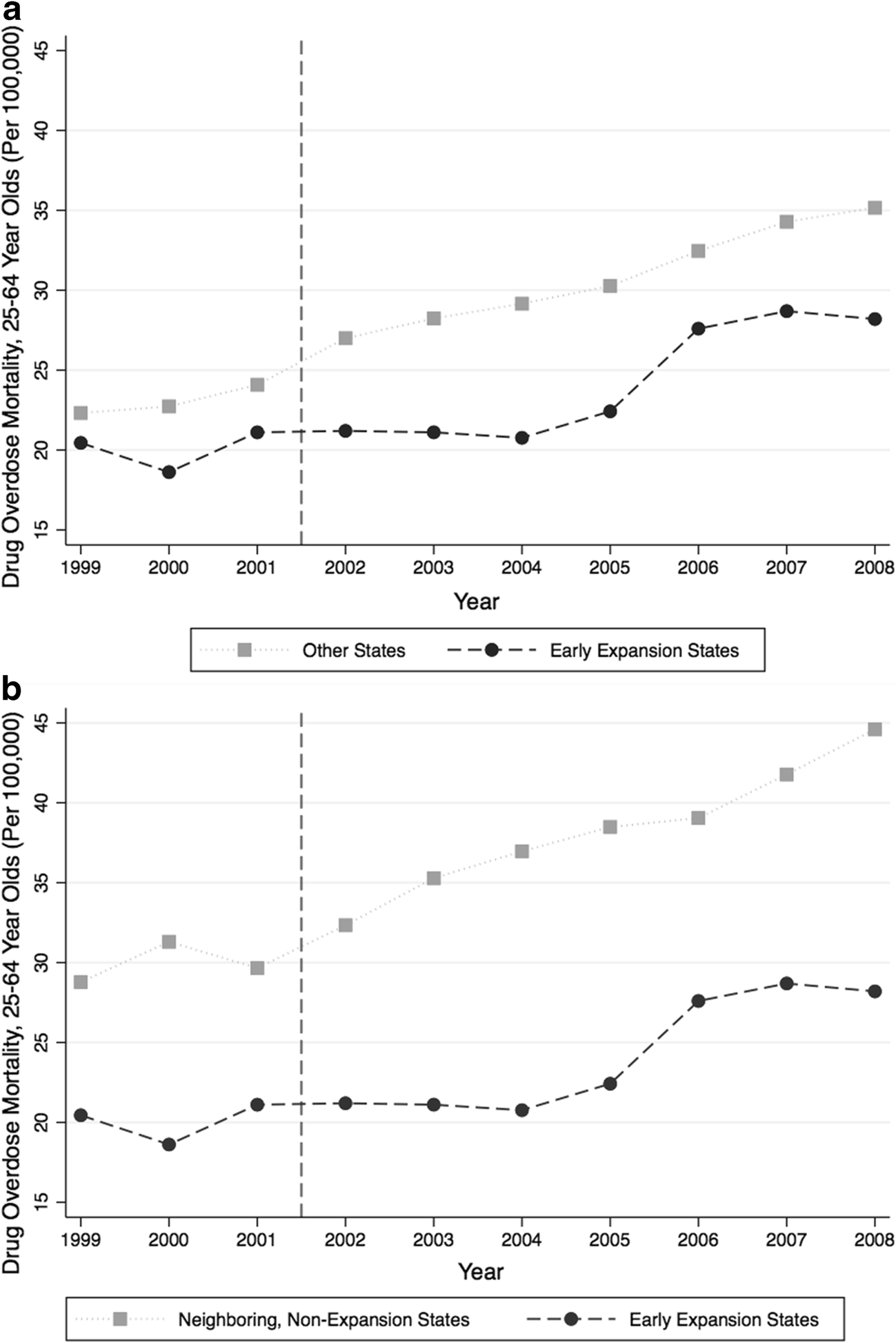
The latest such evidence comes from LDI Senior Fellows Paula Chatterjee and Atheendar Venkataramani, who analyzed trends in drug overdose deaths in three states that expanded Medicaid eligibility before the Affordable Care Act (ACA). Arizona, Maine, and New York all expanded Medicaid program eligibility in the early 2000s. The authors found that rates of drug overdose deaths rose less sharply in these states than in all non-expansion states (Figure 1a), as well as in non-expansion, neighboring states (Figure 1b). The pattern held when they adjusted for secular trends and state-specific social policies, such as minimum wage and welfare and food stamp program generosity.
Source: Journal of General Internal Medicine, September 2018
Assessing the relationship between coverage expansion and overdose deaths is challenging in the midst of a national crisis. Drug overdose mortality rates were already increasing prior to implementation of ACA Medicaid expansions in 2014 (the Centers for Disease Control and Prevention declared prescription opioid overdoses an epidemic in 2011). For this reason, Chatterjee and Venkataramani chose to look at earlier expansions, which took place on the eve of the national epidemic. They estimate that from the time of these expansions through 2008, expansion states averaged four (per 100,000 people) fewer deaths from drug overdose annually than non-expansion states.
Their analysis contributes to the literature debunking claims of a detrimental causal relationship between Medicaid expansion and the opioid epidemic. Another recent study, by Brendan Saloner and colleagues, adds to the evidence base that Medicaid expansion can improve access to treatment for opioid use disorders. The authors compared three states that expanded Medicaid after the ACA (California, Maryland, and Washington) and two states that did not (Florida and Georgia). After adjusting for demographics and secular trends, they found that Medicaid expansion was associated with increased prescriptions for buprenorphine with naloxone, an established best practice treatment for opioid use disorder, without an overall increase in prescriptions for opioid pain relievers.
Taken together, these findings should reassure policymakers that Medicaid expansions are not causing nor fueling the opioid epidemic, but may instead be protective against it.