Health Care Access & Coverage
Blog Post
Surgical Care in Accountable Care Organizations
A Growing Opportunity
Accountable care organizations (ACOs) figure prominently in Medicare’s shift “from volume to value.” Providers in ACOs assume financial accountability for overall quality and costs for a defined patient population, and they earn shared savings for containing spending below a defined benchmark. To date, most ACOs have focused on primary care, outpatient services, and care management for patients with chronic medical conditions, such as diabetes and heart failure. This strategy has yielded some savings, but many ACOs may be missing a critical source of savings: surgical procedures.
Surgical care can have an outsized effect on both quality, such as readmissions, as well as cost. One study estimated that inpatient and outpatient surgery account for half of all Medicare spending. But most ACOs lack comprehensive plans for surgical care, such as strategic referrals to lower-cost, high quality providers. Moreover, many ACO leaders may not even know how much of overall ACO spending is attributable to surgical care.
This lack of knowledge and strategy may explain early evidence that participation in the flagship Medicare Shared Savings Program (MSSP) was not associated with changes in surgical spending.
The policy environment is ripe for change. First, new programs, such as commercial ACOs, Medicaid ACOs, and Medicare’s Next Generation ACO model have increased the number of ACO enrollees and provider participation. Second, the MSSP has moved away from upside-only arrangements, in which participants only earn additional revenue if they produce savings. Looking ahead, participants will be required to assume some downside financial risk for spending that exceeds benchmarks.
Third, policymakers are beginning to recognize the limits of care management programs for patients with chronic medical conditions. As a result, surgical care may represent a new, even greater opportunity, particularly if the volume of procedures performed by ACO-participant surgeons is increasing over time.
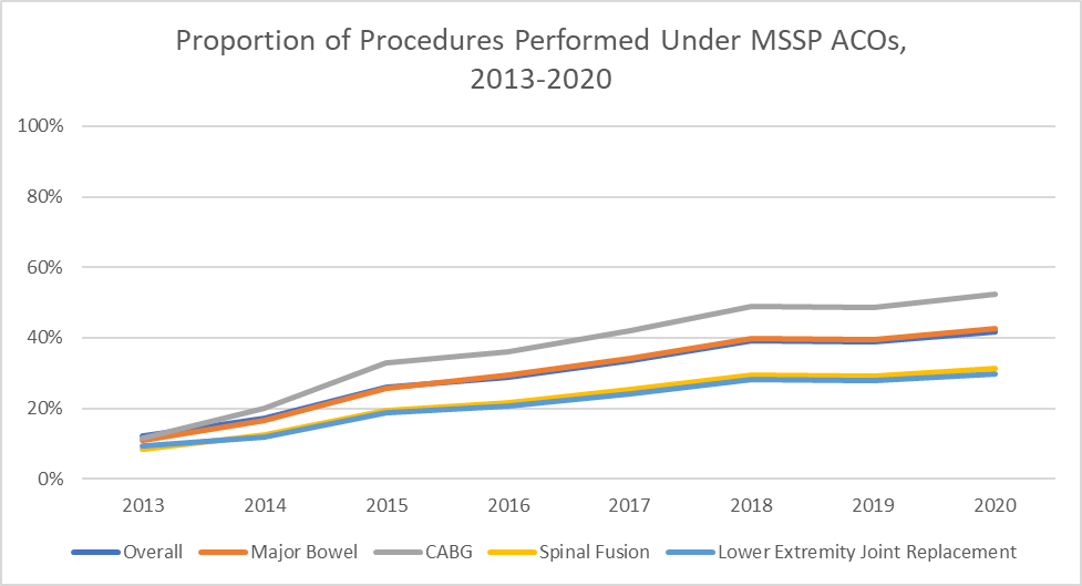
What are the possibilities for surgical savings for ACOs? To estimate this potential, we identified 24 procedures commonly performed among Medicare beneficiaries (Table 1) and used Medicare claims to calculate (2013-2016) or project (2017-2020) the proportion of surgeries performed by ACO-participant surgeons nationwide. We also calculated trends for four procedure types that are both costly and common among older adults: major bowel procedures, coronary artery bypass graft surgery, spinal fusion, and lower extremity joint replacement.
We found that the proportion of procedures performed by MSSP participants has increased over time (Figure 1). Across all 24 procedures, the proportion performed under MSSP ACOs increased from 12% in 2013 to a projected 42% in 2020. Between 2013 and 2020, there were similar trends for major bowel procedures (11% to 43%), coronary artery bypass graft surgery (12% to 52%), spinal fusion (9% to 31%), and lower extremity joint replacement (9% to 30%).
Our analysis underestimates the true magnitude of surgical coverage under ACOs, because we evaluate procedures only under MSSP as a specific program. The proportion of procedures covered would be even greater if we also considered surgeon participation in commercial, Medicaid, and other Medicare ACOs. One caveat of our analysis is that while we evaluated the proportion of cases performed by ACO-participant surgeons, we did not limit procedures to those performed specifically on ACO-attributed beneficiaries. Nonetheless, understanding overall case volume among participating surgeons is itself a critical element of ACO strategy, particularly given the challenges of using attribution information to make real-time decisions (e.g., clinicians frequently do not know which beneficiaries will ultimately be attributed to an ACO at the time of surgery).
In turn, the major finding from this analysis – that an increasing proportion of common surgical procedures are performed by ACO surgeons – has substantial implications. It underscores the growing opportunity that ACO providers may have to manage surgical utilization. As the MSSP program shifts to both upside and downside risk, success in the payment model may hinge on strategic management of surgeries, as well as chronic conditions.