Health Care Access & Coverage
Blog Post
THRIVE: Addressing Patients’ Social Needs after Hospitalization
Academic-clinical partnership develops new pathway
Imagine being discharged from the hospital to a two-room apartment badly in need of repair. Your electricity has been cut off and you can barely remember the discharge instructions. You were told to see a specialist in a week, but it will take you 90 minutes one-way on public transportation to get there. Confused about follow-up and juggling the complexities of life, what do you do?
Patients with significant social needs are at risk for poorer health outcomes after hospital discharge. Often social needs go unaddressed during hospitalization as medical concerns take priority, yet these unaddressed social needs may lead to readmissions or unnecessary emergency department (ED) use. With funding from the Leonard Davis Institute and Penn Center for Health Care Innovation, researchers at Penn Nursing and an interdisciplinary team of clinicians at Penn Presbyterian developed an intervention to improve post-hospitalization outcomes among these patients.
Our team, led by Margo Brooks Carthon, PhD, RN, FAAN and Kendal Williams, MD, MPH, used principles of Design Thinking to understand the needs of socially at-risk patients and to develop a set of solutions centered on their needs. Traditionally, the fields of engineering and business have used Design Thinking as a framework for developing services and products for their end-users. More recently, health care systems have adopted Design Thinking to tackle the growing complexities of health care.
We first spent months “in the field” collecting perspectives of key stakeholders, including patients, clinicians, and hospital administrators to identify obstacles patients faced post-discharge. We learned that patients with concerns related to finances, housing instability, or a lack of transportation felt that they were alone in managing their recovery. Patients with these risk factors were managed differently across units in the hospital, often with limited communication between inpatient and outpatient care providers. From focus groups we found that nurses could easily identify social risk factors, but that lack of time, the prioritization of medical concerns, and a lack of systems in place deterred nurses from addressing patients’ social needs.
To target our intervention, we leveraged data in the electronic health record (EHR) to identify who was most at risk for readmissions. Using machine learning, other statistical techniques, and three months of EHR data, we discovered that:
- Medicaid beneficiaries, who accounted for 24% of admissions to medical services at Penn Presbyterian, represented 45% of patients with one readmission and 64% of patients with multiple readmissions.
- Medicaid beneficiaries who experienced at least one ED visit and had nine or more comorbidities had a 71% probability of readmission, which increased to 92% if the patient was also over age 65.
- The majority (58%) of Medicaid patients went home with no additional supports, with only 22% receiving home care services.
New studies in the Journal of Clinical Nursing and the Journal of Nursing Care Quality describe our work to date. Using what we learned along with the experiences of our interdisciplinary team, we developed a new clinical pathway called THRIVE.
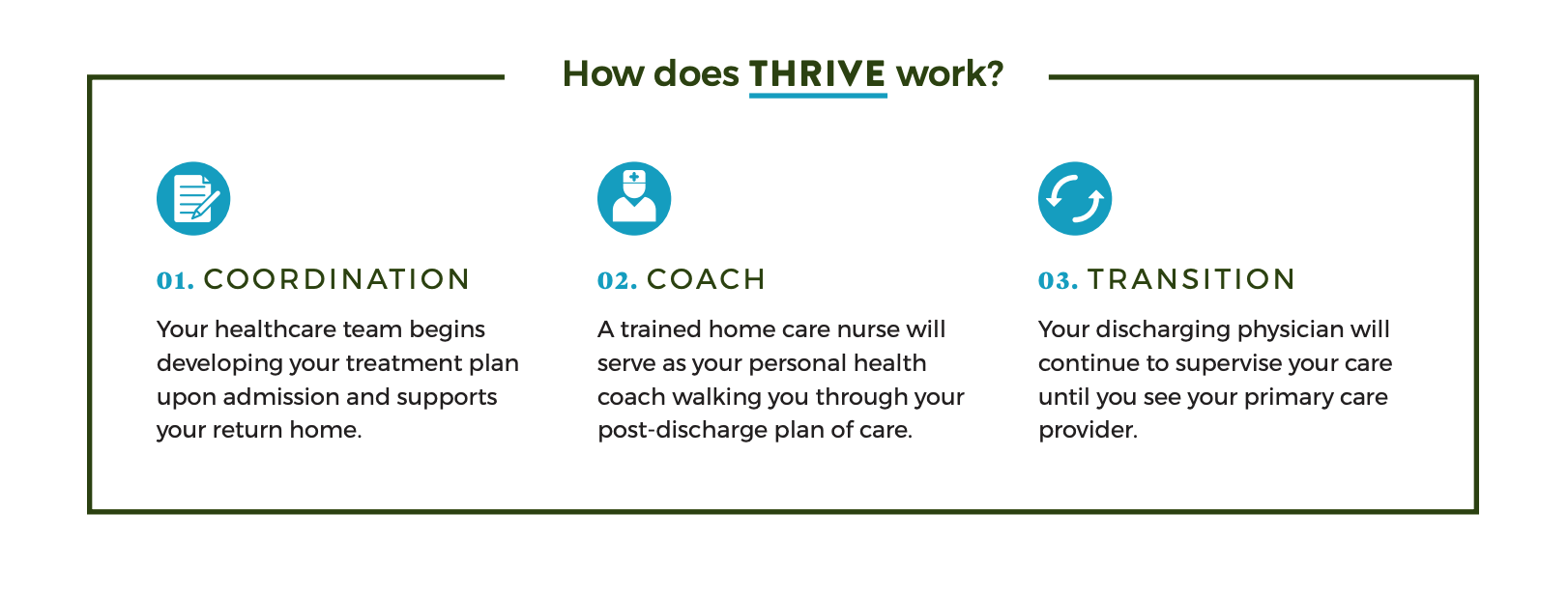
By providing additional supports immediately after discharge, THRIVE is an innovative solution to the current fragmented delivery of care for this high-risk population.

The THRIVE pathway targets medical service patients who reside in Philadelphia, are Medicaid beneficiaries, and have multiple chronic conditions. THRIVE patients are identified during hospital admission and receive a visit from a Penn Care at Home nurse within one day of discharge. During home visits, nurses serve as health coaches and provide patient education, medication reconciliation, and involve other members of the home care team as needed, such as social work and mental health support. The home care nurse has phone access to the discharging attending physician until the patient has a primary care visit or up to one-month post-hospitalization to manage medical concerns as they arise. In the current model of care many socially at-risk patients would not routinely receive a home care referral. Similarly, the current workflow of discharging attendings does not include post-discharge management, nor do home care nurses and discharging physicians communicate routinely.
We are now rapid-cycle testing components of THRIVE. Though the pilot is still underway, home care nurses have already identified social concerns, such as lack of transportation, housing, behavioral health and financial difficulties, and addressed these concerns using home health and community resources. Additionally, communicating with the discharging physician has led to quicker medication reconciliation, medication dose adjustment, and the ability to address medical symptoms in the home. Ultimately, we envision THRIVE will increase continuity across care settings and reduce ED use and readmissions. We continue to seek feedback from patients and clinicians throughout this phase and plan for a more formal program evaluation in the future.
THRIVE was made possible with funding from Penn LDI and the Penn Medicine Center for Health Care Innovation.