Blog Post
Trends in Muscle Relaxant Prescribing
Steep Increase Among Older Adults
As the opioid epidemic rages on, clinicians are looking towards safer medication alternatives for patients with acute and chronic pain. Skeletal Muscle Relaxers (SMRs) are a common opioid substitute for patients with musculoskeletal conditions. Although their use has grown at a rate similar to that of opioids, little is known about their safety and efficacy in treating long-term, chronic pain, particularly for older patients and patients with simultaneous opioid use.
In a retrospective, cross-sectional analysis in JAMA Network Open, LDI fellows Sean Hennessy and Charles Leonard and colleagues Samantha Soprano and Warren Bilker recently examined national trends in outpatient SMR prescriptions from 2005 to 2016. The study included 300 million office visits in which an SMR prescription was initiated or continued.
They found that the number of office visits with an SMR prescription doubled over the last decade, increasing from 15.5 million in 2005 to 30.7 million in 2016. However, the steepest increase was among adults over age 65, for whom SMR visits tripled from 1.3 per 100 visits in 2005 to 4.3 per 100 visits in 2016.
For older adults, office visits with a new SMR prescription remained relatively stable, while office visits with continuing SMR prescriptions increased. This suggests that many older adults may be using SMRs for long-term or chronic pain (Figure 1).
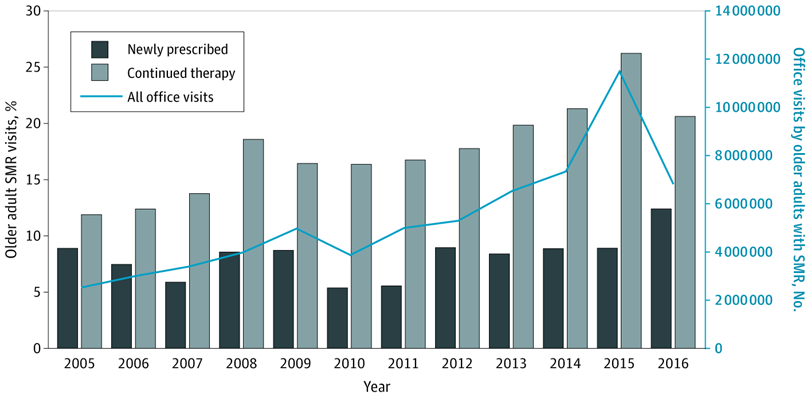
Most new SMR prescriptions were related to back pain and other musculoskeletal conditions. The authors also found that visits with “potentially inappropriate” SMR prescriptions for older adults had doubled from 2.2 million office visits in 2005 to 4.3 million in 2016. Potentially inappropriate medications are those that are best avoided by older adults in many circumstances, including adults with certain conditions or when likely drug-drug interactions exist.
Although SMRs may be considered a promising substitute for opioids, the two drugs are often used concomitantly. The study found that roughly 67% of continued SMR visits recorded simultaneous opioid treatment. This combination increases the risk for serious drug-drug interactions, such as central nervous system depression and opioid overdose.
These trends are alarming and highlight a need for further research into the effects of SMRs and simultaneous opioid and SMR use, particularly in older adults. As physicians continue to prescribe SMRs for acute or chronic pain, they must consider both the short-term risks and benefits, as well as longer-term detriments.
The study, “Assessment of Physician Prescribing of Muscle Relaxants in the United States, 2005-2016” was published in JAMA Network Open on June 24, 2020. Authors include Samantha E. Soprano, Sean Hennessy, Warren B. Bilker, and Charles E. Leonard.