News
An Afternoon with Atul Gawande at Penn Medicine
Leading a Revolution in End-of-Life Care Strategy and Practice

Atul Gawande, Harvard Professor and Executive Director of that university’s Ariadne Labs, addresses an audience of Penn Medicine clinicians and health services researchers. The Penn Health System has recently partnered with Ariadne Labs to implement a new strategy for clinical palliative care.
In 2012 as he was launching a new health services research initiative at Harvard, Atul Gawande reached back into Greek mythology to find an appropriate analogy for the new center. He called it “Ariadne Labs” after the goddess whose gift of a ball of thread enabled the hero Theseus to return safely from a labyrinth after killing the monster Minotaur that threatened the surrounding Aegean Sea community.
The point of course, is that health care is a maze and health services research can be the guiding equivalent of that delicate, ancient twine. The monster at the center of it all is the massively complicated American health care system and Ariadne is using research “threads” to retrieve innovative, evidence-based solutions.
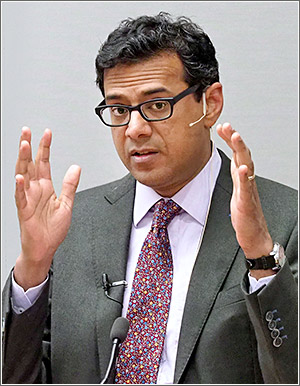
Atul Gawande, MD, MPH, at the University of Pennsylvania Perelman School of Medicine.
In a presentation at the University of Pennsylvania Perelman School of Medicine, which is now working in collaboration with Ariadne Labs, Gawande emphasized that even many in the medical community may not fully comprehend the true complexity of the system in which they work.
Gawande, MD, MPH, is a staff writer at The New Yorker, the author of four books, a surgeon at Brigham and Women’s Hospital, Professor of Health Management at Harvard’s T.H. Chan School of Public Health, and Executive Director of Harvard’s Ariadne Labs, a joint center of Brigham and the Harvard School of Public Health.
Speaking in Penn’s Law Auditorium in an event sponsored by the Penn Medicine Center for Health Care Innovation, Gawande characterized the present era of turmoil in health care as a pivotal point in history. For millennia, he noted, humans lived without scientific medical knowledge and the most learned among them barely knew there were 13 organ systems. But throughout the 20th century and continuing today more than 70,000 human medical conditions have been identified and explosions of scientific discoveries have created more than 6,000 drugs and 4,000 medical and surgical procedures to address that broad array of ailments.
‘Everybody alive’
“Our job now,” Gawande continued, “has become to deploy those thousands of capabilities town by town to every person alive. And I’d argue that there’s nothing mankind has ever attempted that is remotely at that level of complexity. We don’t have any industries that are trying to deliver on 70,000 different services to everybody alive, regardless of their ability to pay, and do it with accuracy, precision and reliability; do it without bankrupting the country; and do it with some humanity.”
One thread of research pursued by Ariadne, which was the focus of much of Gawande’s Penn remarks, is an innovative approach to the clinical planning and execution of care for patients with serious illness. This has traditionally been one of medicine’s most unsettled areas due to clinicians’ often awkward avoidance of the subject, the public’s general dissatisfaction with current end-of-life practices, and policymakers’ concern about the misalignment between the extreme costs and the actual utility of aggressive high-tech treatments in the final months of life.
Gawande, a surgeon, said he came to realize “I didn’t understand how to tackle this area. Twenty-five percent of Medicare spending is in the last year of life, most of it concentrated in the last couple months. We don’t know when that last moment of life will be, so, what could better care be?”
Randomized palliative care study
Written about at length in his magazine articles and books, that question became a research project at Ariadne. Shortly before the Lab launched, Gawande said he was intrigued by the 2010 findings of an end-of-life-care study performed at Massachusetts General Hospital published in the New England Journal of Medicine. That MGH research team randomized two groups of advanced lung cancer patients, with one receiving standard oncologic care and the other getting early intensive palliative care integrated with standard oncologic care.
Large population surveys have found the number of seriously ill people likely to have a conversation with their clinician about their goals for medical care beyond just survival is less than 24%.
with citation
The surprising result was that patients who received the palliative care that included intimate conversations about their well-being, feelings, values, priorities and goals with their clinicians received less aggressive care at the end of their life but survived longer and with higher quality-of-life scores.
The NEJM piece was a lightbulb moment for Gawande. “I could see a couple of options for ‘how do I scale this; how do we deliver this to everybody?’,” he said. “Option one is value the palliative care doctors and the geriatricians. We have fewer people being trained in geriatrics today than we did 20 years ago. That and palliative care are two of the lowest paid professions. We do need more but we’re not on a pathway that would allow us to widely scale.”
‘Beyond just living longer’
“Option two,” he continued, “is to systematically ask people about the priorities they want their medical care to serve beyond just living longer. Learning what their priorities are is a highly technical procedure — you have to ask them. And we don’t ask. Large population surveys have found the number of seriously ill people likely to have a conversation with their clinician about their goals for medical care beyond just survival is less than 24%.”
To better study how to achieve that kind of intimate patient-clinician conversation on a larger scale, Ariadne Labs created the “Serious Illness Care Program,” a system to guide and support new kinds of personally meaningful communications between clinicians and patients. The program is anchored by a guide that clinicians are taught to use to ask key questions that get the conversation started. Its first component is identifying patients at risk of dying.
So far, Gawande said, the most convenient and accurate way for clinicians to do that is to ask themselves, “would I be surprised if this person died within the next year?” If the answer is no, that patient needs to have the conversation.
After that there is a series of questions about many aspects of the person’s life, priorities and goals. And then the clinician can adjust the treatment to be more in alignment with those patient-specific goals.
Training clinicians across the country
In an ongoing randomized trial with the Seriously Illness Care Program at Boston’s Dana-Farber Cancer Institute, Ariadne found a 50% reduction in depression and anxiety among seriously ill patients. Part of that project was the development of a deployable Serious Illness Conversation Training Program that could be used in other interested medical centers. So far, the training program has trained more than 6,500 clinicians and been implemented in 200-300 clinics and 25-30 larger institutions.
Last August, Penn’s Perelman School partnered with Ariadne Labs to begin the training program in its own Cancer Service Line and Palliative Care Programs. Gawande told the Penn audience that implementation by those Penn units is the fastest-spreading he’s seen.
Heading up the team* managing Penn’s partnership and implementation is Nina O’Connor, MD, Director of Palliative Care for the University of Pennsylvania Health System. She said 100 oncology clinicians have been trained to date and the program is on track to train all clinicians in Penn Medicine cancer centers by the end of 2019 as well as all palliative care clinicians.
Penn clinicians ‘initially skeptical’
O’Connor noted that some clinicians were “initially skeptical” but after going through the training rated the experience as “extremely helpful.” She also said the Serious Illness Conversation approach has been found relevant for any patient with a serious life-threatening illness, even those who might eventually be cured.
“The results of really listening to your patients,” Gawande told his Penn audience, “make you realize the goal is not survive at all costs and the goal is not a good death. The goal is a good life all the way to the very end and we providers can enable that. We have experience and we have things to offer and we can match those to what patients want along the way.”
And, he suggested, despite the sometimes gloomy essence of the work, connecting and bonding in a more empathetic way with seriously ill patients has its surprisingly fulfilling and often humorous moments. Recounting an event he captured in one of his books, Gawande told the story of a terminally ill patient who engaged in the “conversation” and was asked to define his specific priorities as his condition continued to worsen.
“Well, if I can eat chocolate ice cream and watch football on television, that would be good enough for me. If I can do that, keep me going. If I can’t, let me go,” the patient said.
“It was the best living will ever,” Gawande told the Penn audience.