News
Photo Page: Closing the LDI 50th Anniversary Symposium
Last Day Highlights Panels of Top Health Care Authorities Looking to The Future
PHILADELPHIA (Oct.6, 2017) — The second day of the Leonard Davis Institute of Health Economics 50th Anniversary Symposium was highlighted by a “What is the Future of Health Care?” plenary featuring four of the country’s top authorities on health care policy. Speaking before a standing-room-only audience in the ballroom of the Inn at Penn Conference Center were (above, l to r on stage) David Brailer, MD, PhD, who served as the country’s first National Health Information Technology Coordinator; Ezekiel Emanuel, MD, PhD, a former White House Special Advisor for Health Policy and one of the architects of the Affordable Care Act; Mark Pauly, PhD, a Wharton School professor and nationally renowned health economist; and Andrew Slavitt, MBA, former Administrator of the Centers for Medicare and Medicaid Services (CMS).
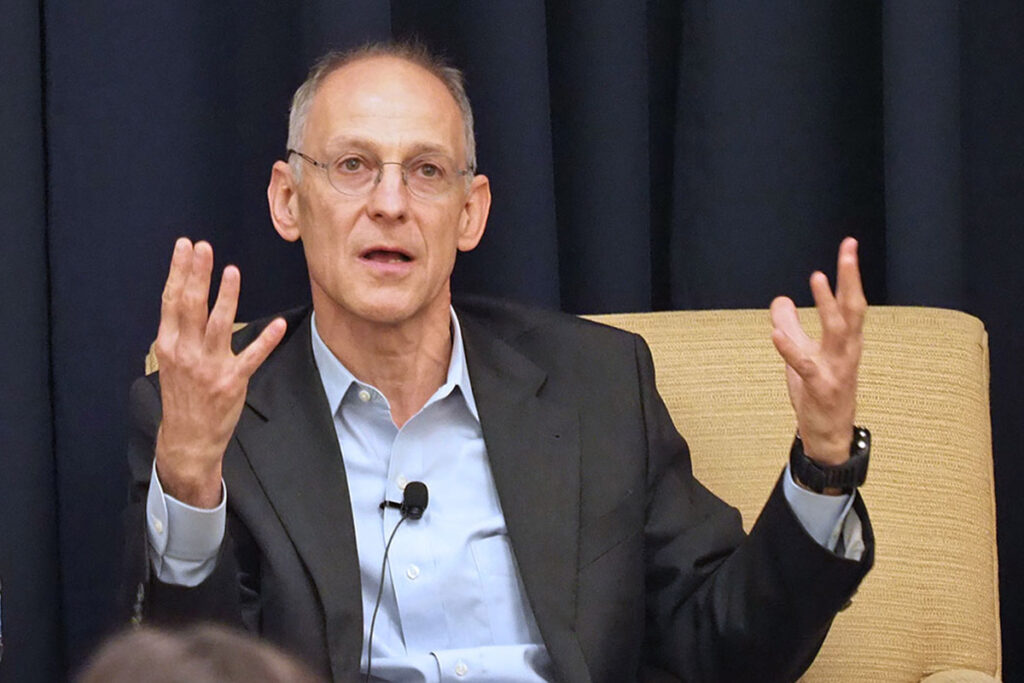
On Capitol Hill as the symposium convened, multiple hurried attempts to repeal the ACA had failed, leaving a slow-moving stalemate as the current administration used what executive powers it could to weaken or eliminate financial supports for the ACA. Moderator David Brailer characterized the situation as “a guessing game” with no direction or resolution in sight and asked panelists for their take on the situation. Ezekiel Emanuel (above, left), now a University of Pennsylvania Vice Provost, said that despite federal government actions, the private sector and insurance industry continued their own push for sweeping payment system changes aimed at achieving a higher value system that would likely continue, albeit more slowly. Andrew Slavitt (above, right) was not as optimistic. “If you’re 40% of the poverty level, you’re being priced out of the market,” he said. “I think we will end up with a very politically important, isolated group of people that are increasingly angry and upset and demanding that something be done about the law.”
In their closing remarks, LDI Executive Director Daniel Polsky, PhD (above, left), and Penn President Amy Gutmann (above, right), looked beyond the current political debates about health care, emphasizing the importance of maintaining and broadening a national community of health services and policy researchers whose work is critical to the process of improving health care.
In his presentation, Penn Law School Dean Theodore Ruger, JD (above, left), emphasized the crucial importance of scientific gatherings. “I look around the room and I see people who I work with every day as well as people who I’ve collaborated with on health law projects over a decade ago and haven’t seen since because they live in other parts of the country,” he said from the podium. “Indeed this exemplifies what is best about LDI as an ongoing convening space, enabling people from different disciplines to convene from across this campus, drawing leading experts in health care, policy, economics, law and other fields together to a central point where we can discuss the health care system issues using our unique disciplinary perspectives.” Above, right, Director of Penn’s Center for Health Incentives and Behavioral Economics (CHIBE) and LDI Senior Fellow Kevin Volpp, MD, PhD (above, right), discussed one of those issues. He pointed out that over the last 50 years, at the same time it became the country with the highest health care costs, the U.S. dropped to the 26th rank in life expectancy among the world’s industrialized nations.
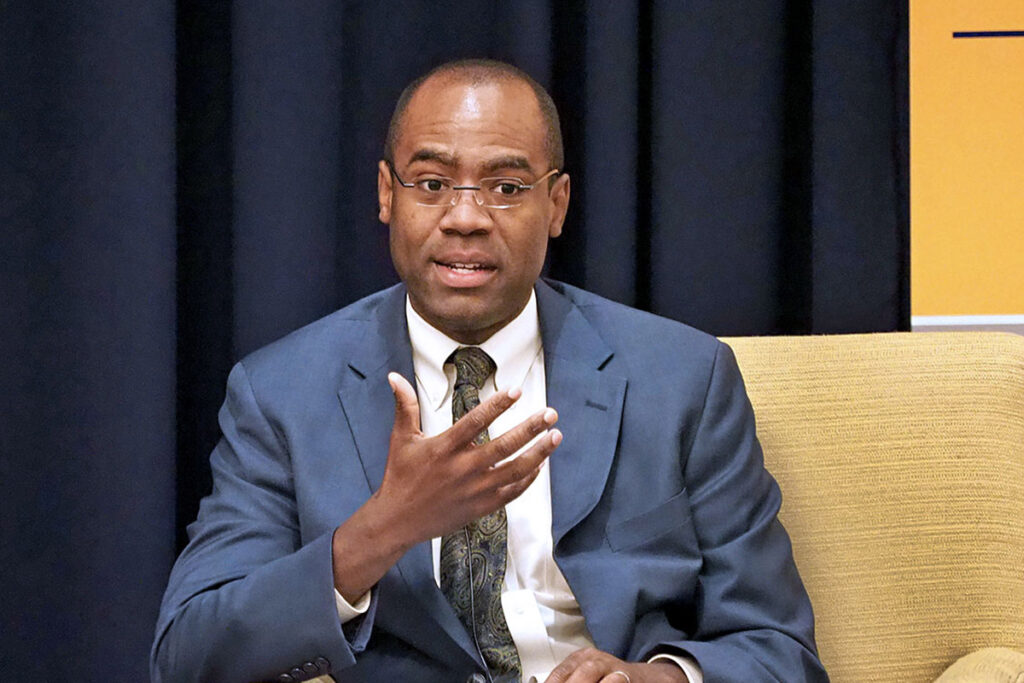
In a “State Health Policy Challenges and Innovations” panel moderated by Julian Harris, MD, MBA (above, left), Senior VP for Strategic Operations at Cigna, Louisiana Secretary of Health Rebekah Gee, MD, MPH, pulled no punches. “Recent discussions on health reform are not addressing the real problems in health care,” she said. “These are: poor outcomes, increasing costs, lack of patient engagement, and giving states REAL flexibility, like negotiating drug prices, or being able to work with Medicare to not pay for low value services, or shifting more spending toward the social determinants of health because ZIP codes mean more to our health than our genetic code. Those are the types of discussions we need to have. Instead, we’re talking about major cuts without any sort of significant structural reform.”
Former Secretary of Human Services in Pennsylvania and currently a special advisor to the governor, panelist Theodore Dallas, MBA (above, left), underwent surgery and radiation therapy for throat cancer during the summer. “As I was getting world-class treatment here at Penn,” he told the audience from his seat on the “State Health Policy Challenges” panel, “the thing I kept thinking about was ‘what if I didn’t have insurance?’ What if I was on Medicaid?’ It provided a new dimension in my understanding of what people go through in the health care system.” Above, right, Julie Sochalski, PhD, RN, FAAN, Associate Dean for Academic Programs at Penn’s School of Nursing and a researcher nationally recognized as an expert in health policy and health care workforce issues, spoke about the importance of research collaboration in the future of health care. “I look around the room and see partnerships between people like Mary Naylor and Mark Pauly that gave us an opportunity to take something like the transitional care model, incorporate it into Medicare, and make a difference in one of the biggest areas of hospital costs,” she said.
Sitting on the “Health Systems and Payment Reform: Managing Risk, Harnessing Opportunity” panel (above, left) are Penn Medicine CEO and LDI Senior Fellow Ralph Muller, MA, and Vizient Research Institute Executive Director Tom Robertson, MBA. Above, right, on the “Risk Adjustment and Measuring Quality” panel moderated by Penn Medicine’s Lee Fleisher, MD, and Jeffrey Silber, MD, PhD, are (l to r) Shantanu Agrawal, MD, MPhil, President of the National Quality Forum; Rachel Werner, MD, PhD, Penn Professor of Medicine; and Pierre Yong, MD, MPH, MSHP, Director of Quality Measurement at the Centers for Medicare and Medicaid Services (CMS); and Silber, Professor of both Pediatrics at Penn Medicine and Health Care Management at the Wharton School.
Jalpa Doshi, PhD (above, left), Professor of Medicine at the Perelman Medical School and Director of Value-Based Insurance Design Initiatives at CHIBE, moderated the “Value Frameworks in the U.S.” panel. Above, right, panelist Michael Aberman, MD, MBA, President and CEO of Quentis Therapeutics, a biotech company focused on cancer drug development.
Above, left, economist Mark Pauly in a spirited discussion with James Thomas, MD, MBA, an interventional radiologist and Immediate Past President of the Montgomery County Medical Society of Pennsylvania. Above, right, LDI Adjunct Senior Fellow and Principal in the Wharton-affiliated Center for Applied Research (CFAR) Thomas Gilmore chats with Lawton (Rob) Burns, PhD, MBA, Wharton School Professor of Health Care Management, and LDI Senior Fellow.
Catching up, former Penn colleagues Katrina Armstrong, MD, MSCE, and Arnold (Skip) Rosoff, JD, chat in the Inn at Penn’s Living Room lounge (above, left). Armstrong, a Professor of Clinical Medicine at Harvard Medical School and Physician-in-Chief at Massachusetts General Hospital, was previously the Chief of Penn Medicine’s Division of General Internal Medicine. Rosoff is Professor Emeritus of Legal Studies and Health Care Management at the Wharton School. Above, right, The “Drug Pricing” panel (l to r) Brian Corvino, MBA, SVP of Decision Resources Group; Jeffrey Marrazzo, MBA, MPA, Spark Therapeutics; Scott Ramsey, MD, PhD, Director of the Fred Hutchinson Cancer Center; and moderator Patricia Danzon, PhD, Wharton Professor of Health Care Management.