
Only One in Four High-Risk Rural Births Get Appropriate Hospital Care
A Multi-State Study Finds That Parents Often Travel 60+ Miles—With Distance, Insurance, and Race Driving Gaps in Maternal Care
News
A new University of Pennsylvania study of inpatient maternity care incident notes has found that communications failures among members of the clinical team were more common for Black women.
The work was led by LDI Senior Fellows Rebecca Clark, PhD, RN, FAAN, Assistant Professor of Family and Community Health at Penn’s School of Nursing and nurse scientist at Pennsylvania Hospital and Rebecca Hamm, MD, MSCE, an Assistant Professor of Obstetrics and Gynecology at Penn’s Perelman School of Medicine. Kathy Sliwinski, PhD, RN, Tamar Klaiman, PhD, MPH, and Emilia Flores, PhD, MS, RN, were critical members of the team.
Clark said that while other studies had focused on provider notes entered in electronic health records (EHR), she was unaware of any similar study in the maternity literature that had focused on incident reports as their data source.

All hospitals are required by the Joint Commission to have incident reporting systems in place. These systems, usually electronic and distinct from the electronic health record (EHR), are designed to help staff raise safety concerns to leadership. The types of issues reported can range widely—from improperly sterilized surgical tools and malfunctioning equipment to unprofessional behavior among staff and negative patient outcomes.
This study analyzed anonymized hospital incident reports to understand communications failures in the women’s health units (antepartum, labor and delivery, and postpartum) at a large urban health center and how those were related to severe maternal morbidity (SMM) outcomes.
Patients experiencing SMM have one or more unexpected and serious health complications during pregnancy, childbirth, or the postpartum period that could result in significant short- or long-term health consequences.
The study found that Black women represented 28% of the births in the 2019–2022 period but were the subject of 38% of the incident reports. Most of the communication failures detailed in the incident reports occurred within the clinical team rather than with patients. In other words, most of the communication failures occurring around Black women did not directly involve them but were happening among the healthcare team members taking care of them.

The authors explored communication failures overall, but also by patient race/ethnicity and SMM status. They found that the most common communication failures around SMM events were those of omission (for instance, missing sharing a critical piece of information about the patient’s health history).
Published in BMJ Open Quality, the paper notes, “A significant body of literature indicates that communication between clinicians and Black women is a significant problem, with clinicians not listening to Black women or communicating in a respectful, person-centered manner.” It also points out that “the specific kinds of communication failures associated with poor outcomes and inequities are less well understood.”
Black women were disproportionately represented among this study’s incident reports for different kinds of communication failures compared to White women. Black women, however, were also disproportionately represented among health equity communication codes (for instance, “against medical advice” incidents) and White women were disproportionately represented among incident reports that were examples of positive communication.
The study identified four specific areas of concern found in the incident notes:
• Contextual failures, such as not reporting changes in blood pressure after delivery to a physician or midwife.
• Conceptual failures, including a lack of shared understanding, such as failing to follow protocols for epidural insertions.
• Sociotechnical failures, involving workflow issues—for example, transferring a patient with multiple health concerns to the postpartum floor without requesting a bed.
• Researcher-defined equity concerns, such as situations where women felt they had no choice but to leave the hospital early to care for children at home, without support to do so safely.
The authors wrote, “We found that communication issues reported in incident reports were predominantly interpersonal within the health care team and rarely involved patients or technology. … While attention has focused on communication failures between the health care team members and patients, less has been paid to how racism—or other forms of bias—function in communication within the health care team. This biased communication can occur within the health care team toward another member of the team, as well as within the health care team surrounding a patient.”
“Incident reports provide an opportunity for health systems to leverage their data to more accurately pinpoint opportunities for improvement,” said Clark. “Our findings suggest that to achieve equity and address disparities, we can focus on improving communication within the health care team, especially around caring for patients from vulnerable communities.”
The paper concluded that “efforts to improve health care team communication might include regular multidisciplinary review of policies and procedures to increase shared understanding, simulation of communication in emergency and hand-off situations, and standardization of clinical procedures.”


A Multi-State Study Finds That Parents Often Travel 60+ Miles—With Distance, Insurance, and Race Driving Gaps in Maternal Care

Former CMMI Leader Liz Fowler Cites Rigid Federal Scoring Rules and Bureaucratic Impatience for Pilot Failures

A Major European–U.S. Hospital Study Finds That Changing How Hospitals Are Organized Reduces Burnout and Turnover While Improving Care Quality

An LDI Fellow Who Helped Architect the ACA Highlights Progress on Primary Care Payment Reform and the Expansion of Site-Neutral Reimbursement Policies

Penn LDI Senior Fellow Dominic Sisti Cites “Alarming Levels”
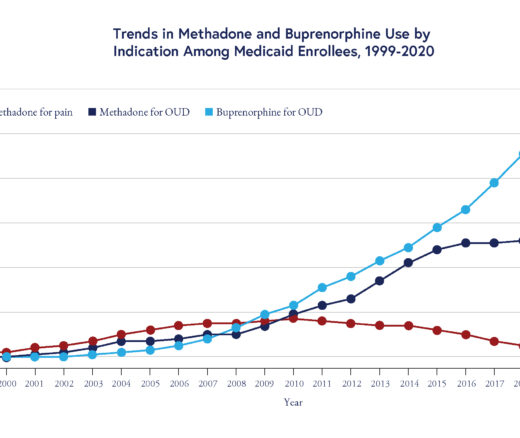
Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication