
A Bold Plan to Fix Medicaid
Democrats Must Go Beyond Reversing Trump-Era Cuts With a New Strategy to Streamline Coverage, Reduce Waste, and Expand Access to Medicaid
Blog Post
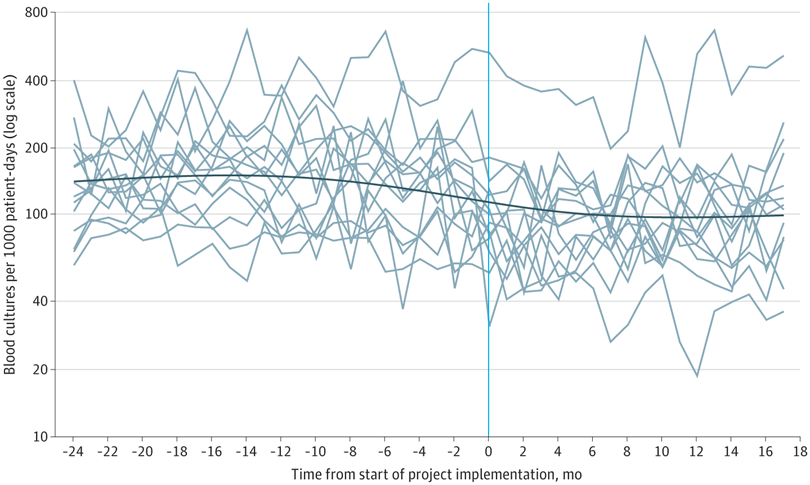
Blood culture tests are commonly overused in the pediatric intensive care unit, a practice that leads to unnecessary antibiotic use and contributes to antibiotic resistance. Optimizing blood culture practices through diagnostic stewardship may reduce unnecessary blood cultures and antibiotics.
In a new study in JAMA Pediatrics, my coauthors and I report on a multicenter diagnostic stewardship intervention designed to optimize and reduce the use of blood cultures for critically ill children. The intervention involved 14 pediatric ICUs—all members of a collaborative called Bright STAR. When we assessed the effects of the Bright STAR intervention in these ICUs after 24 months, we found it reduced blood cultures by 33% and antibiotic use by 13% without changing safety or balancing metrics, such as mortality or sepsis.
How did we do it? We used human factors engineering to understand blood culture practices across the study hospitals, and then we developed site-specific new clinical tools informed by key stakeholder perspectives and unique patient needs. Throughout the project, we assessed elements of both work system factors and quality improvement infrastructure, and we used customized implementation strategies to integrate the clinical tools at each site.
This study points to a promising strategy to change clinical practice, including one of the hardest changes to make—stopping old habits.
The study, “Association of Diagnostic Stewardship for Blood Cultures in Critically Ill Children With Culture Rates, Antibiotic Use, and Patient Outcomes,” was published May 2, 2022, in JAMA Pediatrics. Authors include Charlotte Z Woods-Hill, Elizabeth A. Colantuoni, Danielle W. Koontz, Annie Voskertchian, Anping Xie, Cary Thurm, Marlene R. Miller, James C. Fackler, Aaron M. Milstone, and the Bright STAR authorship group.


Democrats Must Go Beyond Reversing Trump-Era Cuts With a New Strategy to Streamline Coverage, Reduce Waste, and Expand Access to Medicaid

Food-Insecure Cancer Survivors Live Shorter Lives, Especially if They Can’t Use Federal Programs Like SNAP

Memo: Delivered to the U.S. Food and Drug Administration (FDA)

A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike

Stable Payments Improved Margins But Not Liquidity, New LDI Analysis Finds

LDI Senior Fellow Cited for “Significant Contributions” in Research

Outdated Laws Target Black and Queer Lives in Over 30 States, Fueling a Deadly Disease

Selected for Current and Future Research in the Science of Amputee Care