Blog Post
Do Incentive Payments Improve Home-Based Primary Care?
Evidence from the Independence at Home Demonstration
After five years, a small experiment to improve care for frail elderly patients receiving primary care at home has delivered some savings to Medicare—although it might be too small to know for sure. Authorized by the Affordable Care Act, the Independence at Home (IAH) Demonstration is part of a broader strategy of testing innovative ways to pay for value in health care—tying additional payment to higher quality care and cutting wasteful spending.
The IAH Demonstration allows home-based primary care practices to receive additional shared savings payments to care for frail, high-cost patients. Beneficiaries must have two or more chronic conditions, require assistance for at least two activities of daily living, and have had a hospitalization and rehabilitative service in the prior 12 months. In short, the program is targeting a small subset of Medicare beneficiaries (6%), who make up a disproportionate share (30%) of total Medicare spending. Practices earn bonus payments based on a shared savings formula, but only if they meet quality standards for at least three of six measures. The case for IAH is intuitive: home-based primary care may allow providers to spend more time with patients, provide accurate assessments at home, and deliver more convenient care at lower cost.
By design, the demonstration is relatively small in scope. At the start of the program in 2012, Congress limited total enrollment to 10,000 patients, and 17 provider groups participated. In 2015 the program was set to expire, but legislators granted a two-year extension/expansion, followed by another in 2018, which increased the demonstration size to 15,000 but did not increase the number of provider groups being evaluated. In 2019, 14 provider groups remained, with 15,000 Medicare beneficiaries enrolled.
Evaluation findings
So far, two independent evaluations required by Congress suggest positive results in terms of utilization and quality. The first evaluation looked at three years of cumulative program data and found statistically significant, modest decreases in emergency department visits, unplanned hospital readmissions, and the number of preventable hospital admissions. A second evaluation found a similar decline in potentially avoidable hospitalizations and emergency department visits. In both evaluations, mortality remained unchanged and patient satisfaction was high.
But the story on cost savings is murkier. CMS produces annual reports of savings returned to IAH practices. In the fifth program year, CMS reported that per beneficiary spending was 8.4% below benchmark, resulting in $33.5 million in savings and aggregate bonus payments of almost $7 million to eight provider groups. If one were to sum the total savings from each of the five evaluation years, it would suggest the program generated over $100 million in cost reductions. However, Medicare’s mechanism for evaluation changed substantially over time in dialogue with program participants. As a result, the savings aren’t comparable year over year.
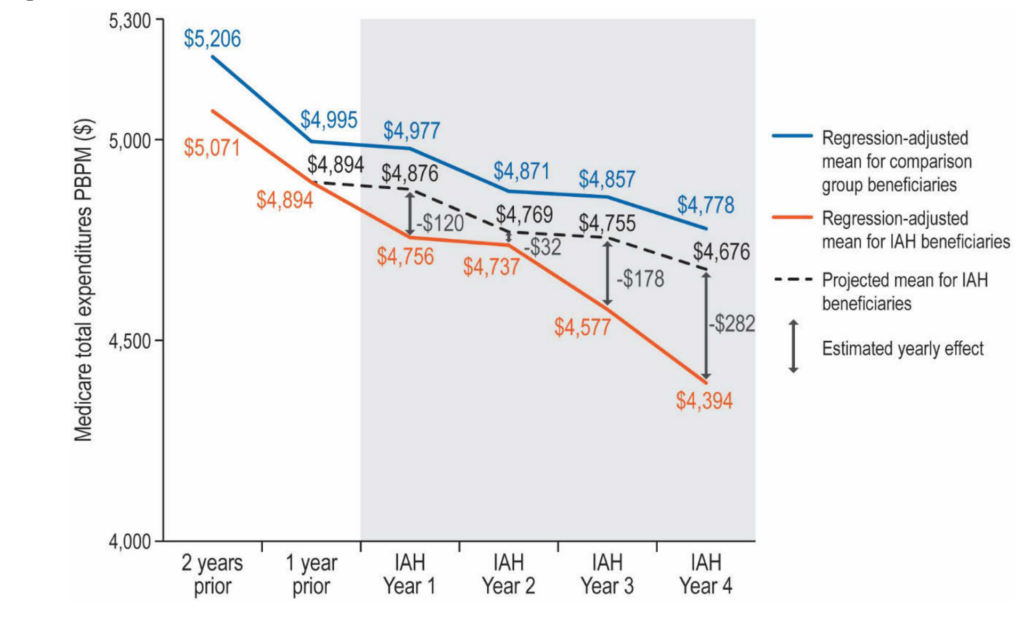
In contrast, the independent evaluations required by Congress found less impressive results. The three-year evaluation found a 2.5% reduction in costs per beneficiary per month, but the results were not statistically significant. The four-year evaluation also found that per beneficiary expenditures had decreased, by 3.7%, which again did not meet the threshold for statistical significance. However, as the evaluators noted, the cost estimates for the IAH group appeared to decrease more over time relative to the comparison group, with Year 4 showing the largest decrease: from $120 per beneficiary per month in Year 1 to $282 in Year 4 (see figure below). Furthermore, both evaluations found that independent practices outperformed academic medical centers on most measures, achieving larger, statistically significant savings. But because of the considerable uncertainty around these estimates, these findings cannot be considered conclusive evidence of cost savings for the program overall.
The diverging results are not necessarily surprising. Determining causality within the IAH program has proven exceedingly difficult for evaluators. The IAH demonstration targets a small, expensive, and difficult to evaluate population. High-risk patients have substantial random fluctuations in expenditures and outcomes, and many of those fluctuations also affect eligibility for the IAH program (e.g., hospitalizations). Therefore, it is difficult to parse a clear upshot from these evaluations. While the evidence on cost is equivocal, some utilization measures improved without adverse effects regarding mortality, patient satisfaction, or long-term care placements. At the very least, IAH practices received shared savings without harming the quality of care.
Future of IAH
IAH expires at the end of 2020, and Congress must decide whether to extend it (for the third time), end it, or expand it to more practices. Two bills in Congress—one offering a temporary extension and another to take the program nationally—remain in committee. In retrospect, the lack of clarity with regards to IAH’s effect on cost could have been foreseen because the program was initially underpowered to detect modest savings.
Going forward, there is a case to be made for expanding the IAH program. The program did not have adverse effects on patient care and may have improved quality. The utilization data suggests savings could materialize. However, policymakers should pay close attention to how the program is expanded—with an eye towards more reliable evaluation. This could include ensuring that the number of patients across the program is large enough to adequately detect cost savings, as well as focusing the program on independent practices, which have shown the greatest promise so far. The tantalizing potential of significant Medicare savings in this high-risk, high-cost group should not be dismissed lightly.