
Inside Medicare’s Stalled Shift to Value-Based Care
Former CMMI Leader Liz Fowler Cites Rigid Federal Scoring Rules and Bureaucratic Impatience for Pilot Failures
News | Video
Begun as an egalitarian crusade of the Truman administration in 1946 to create a loose network of small hospitals for populations across the country’s remote regions, the rural hospital movement has never faced threats to its existence as dire as those confronting it today. And that situation continues to worsen as fragmented—and often contradictory—federal and state efforts to prop up the system have not succeeded.
In an assessment issued in May of last year, the U.S. Government Accountability Office (GAO) estimated that 20% of the U.S. population—or 60 million people—live in these rural areas and generally experience worse health outcomes than urban residents. For instance, the GAO pointed out, those rural communities have higher rates of maternal mortality and other serious adverse health outcomes.
In a national report earlier this year, the health care consulting company Chartis noted “America’s rural health safety net has been in crisis mode for nearly 15 years. Rural hospital closures, decreasing reimbursements, declining operating margins, and staff shortages have all coalesced to undermine the delivery of care in communities whose populations are older, less healthy, and less affluent. The mission of the safety net to serve under-resourced communities is unraveling.”
Against this background, the University of Pennsylvania’s Leonard Davis Institute of Health Economics (LDI) convened an April 19 virtual seminar bringing together five top experts to explore the issues and potential alternative solutions to this crisis.

As she opened the session, LDI Executive Director Rachel M. Werner, MD, PhD, explained, “Since 2005, more than 190 rural hospitals have closed across the United States, and many more are in danger of closing because of financial shortfalls. This problem is only getting worse, with a recent report finding that half of rural hospitals lost more money in the past year, up from 43% in the previous year.”
The panelists included Paula Chatterjee, MD, MPH, of the Perelman School of Medicine whose research focuses on the financing, quality, and outcomes of the national health care safety-net; Ramona Hicks, RN, CEO of Coulee Medical Center, a 25-bed rural hospital that serves a remote five-county area of Washington state that includes the Confederated Tribes of the Colville Reservation; Tony Leys, Rural Editor and Correspondent of KFF Health News; and Harold Miller, MS, President and CEO of the Center for Healthcare Quality and Payment Reform.
Their overall message was that the driving central force behind hospitals’ problems is a lack of coherent and adequate national funding policies exacerbated by private insurers unwillingness to reimburse for the full cost of procedures and Medicare Advantage’s prior authorization policies.
A fragmented tangle of federal and state programs has emerged to address this rural hospital funding problem in recent years, but each in their own way. These include:
These programs don’t seem to have fully considered the fact that insurers are not paying for the full costs of procedures in a rural hospital because procedures done on a much smaller patient cohort don’t generate the revenue needed to cover a facility’s fixed costs. For this reason, panelists concurred that rural hospitals need to be paid more per procedure than larger hospitals just to break even and keep the lights on.

“There’s a number of myths about rural hospitals,” said Miller. “The most problematic of which is the idea that their closing has something to do with low payments from Medicare and Medicaid, or lack of Medicaid expansion. The reality is that it’s low payments from private insurance plans that are causing the problem in rural hospitals. There’s a widely held belief that both large and small hospitals get higher payment from private insurance plans than Medicare and Medicaid. But the exact opposite is true for a lot of small rural hospitals. They get paid less by private insurance plans than Medicare, and, in some cases, even Medicaid.”
“The other part of the myth is that the vast majority of the patients at rural hospitals are all Medicare and Medicaid patients,” Miller continued. “But, in fact, 40% to 50% of the services that rural hospitals deliver go to privately insured patients. So, if the rural hospital is being underpaid for half of its patients, it’s not surprising that it’s going to lose money.”

Speaking from experience within her own rural hospital, Hicks said, “The most disturbing trend we’re seeing is the denial by commercial insurers. It’s overwhelming to the point that we’ve just purchased software to track and document it. In addition, that trend is accompanied by the trend of Medicare Advantage that is sold to people for services that are 100 miles away, but they don’t understand that. They got a $100 food card for signing up and it’s very difficult for us to talk to them and tell them that their service in our hospital won’t be paid for by their coverage. In terms of rural hospital issues, insurance is the huge piece that needs to be talked about and addressed in a meaningful way.”
Another issue impacting rural hospitals is “rural bypass,” or the decision of substantial numbers of rural patients to seek their care at a distant larger hospital instead of the rural hospital closer to home.

“Some studies on this are saying 25% to 50% of rural patients are bypassing their local hospital,” said Chatterjee. “Qualitative studies show even higher rates of 60% to 70%, so the actual range of this is hard to pin down. In some small qualitative studies where we talked with rural people, they’ve said they are basically concerned about limited services, even if the local hospital provides those services.”
Leys pointed to the impact of regional health systems’ powerful marketing campaigns. “It depends on the market and distance from a rural hospital, but if you’re within fairly easy driving distance and the city hospital is marketing like crazy, they’re doing that for a reason,” he said. “They spend advertising money at a scale that the smaller hospital is not going to be able to compete with.”
Chatterjee noted the proven retention power of strong connections to local primary care. “One of the most interesting and valuable pieces of data we have on rural bypass is that when patients have strong primary care relationships close by, they are more likely to go to their local hospital,” she said. “That is something heavily undervalued right now. When patients feel trust and have strong relationships and continuity of care in the local outpatient setting, it matters in their decisions about the inpatient setting. Having policy along this continuum is supported by evidence but that’s somewhat missing from the conversation.”
Several of the recent federal programs that have been created to address rural hospitals’ problems are solutions that don’t quite seem to fit. One of those is the Centers for Medicare and Medicaid Services (CMS) Rural Emergency Hospital program that attempts to address the insufficient funds rural hospital have for inpatient services by providing incentives for those hospitals to close their inpatient units.
Chatterjee explained, “The program allows rural hospitals to power down their inpatient operations and then maintain themselves as a freestanding rural emergency department and outpatient services department. In exchange for doing that, Medicare provides them with a ‘facility fee’ and a payment for providing outpatient services.”

“This has been highly controversial for a variety of reasons,” Chatterjee continued. “Many are asking, ‘Why are we just continuing to withdraw clinical services from rural areas? Why is that the answer?’ Why isn’t the answer to give additional support to these facilities, to allow those services to thrive, proliferate and serve patients?’ A broader focus is required for keeping rural health care open that recognizes that both the hospital and the rural community around it need to be targeted for rural community-level interventions. A rural health care system that is viable and serves its patients best, cannot be separated from helping rural communities thrive.”
Leys pointed out that the ability of rural hospitals to provide comprehensive health care in their areas after they simultaneously close their inpatient, or OBGYN units varies. For instance, some rural hospitals have integrated with distant large healthcare systems to which they can send patients who need the services that they no longer provide.
“If you’re a small hospital that’s connected to a health system with a much bigger hospital down the road, that seems more doable,” Leys said. “You could set up a pathway where people could easily go back and forth, with both the rural hospital and the distant larger one having access to the same medical records. But if you’re a very isolated, independent hospital, as many of these are, that is much harder to do.”
“Another consideration is our experience with the pandemic,” Leys continued. “A lot of these rural hospitals that usually had only one or two inpatients at night suddenly had a whole lot more coming in with COVID-19. The point is that their inpatient capabilities suddenly became really important because the medical centers they usually transferred patients to were jammed and begging them to hold on to as many patients as they could. I’ve talked to hospital administrators who ask, ‘If we close these rural hospital inpatient units, what are we going to do when another pandemic or national emergency comes along?'”
Miller pointed out that it’s not well appreciated that in many areas, the rural hospital is the health system. When it closes, “communities lose everthing.”
“We need to change the perceptions about these things if we’re going to get to genuine solutions for rural hospitals,” Miller said. “We need to be thinking about a different approach to paying rural hospitals that’s a combination of two different kinds of payments. The first is a ‘standby capacity payment’ from all payers that supports a minimum fixed cost for essential services like an emergency department or an OB-GYN unit. The second is the payment of smaller fees for individual services. That would also then make the care at a small rural hospital more affordable for individuals in the community because they’re not having to pay for all of those fixed costs every time they go and get a test or have a visit there. This combination of standby capacity payments and service fees would be a much better payment system than any of the things that have been tried so far.”

.

Former CMMI Leader Liz Fowler Cites Rigid Federal Scoring Rules and Bureaucratic Impatience for Pilot Failures

A Major European–U.S. Hospital Study Finds That Changing How Hospitals Are Organized Reduces Burnout and Turnover While Improving Care Quality

Penn LDI Senior Fellow Dominic Sisti Cites “Alarming Levels”

Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
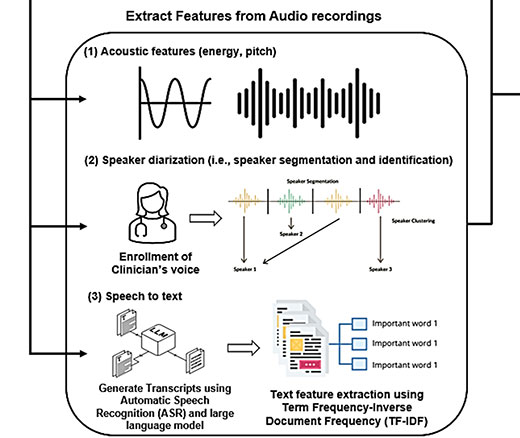
Researchers Use AI to Analyze Patient Phone Calls for Vocal Cues Predicting Palliative Care Acceptance

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print