Brief
Health Screening for Emerging and Non-Communicable Disease Burdens Among the Global Poor
Evidence From Sub-Saharan Africa

Key Findings
Among adults in rural Malawi, population health screening for high blood pressure (BP) led to a 22-percentage point drop in the likelihood of being hypertensive four years later. Individuals with elevated BP received a referral letter upon initial screening; at follow-up, they had lower BP and higher self-reported mental health than individuals with similar BP who were just below the threshold for referral. Population health screenings can reduce the burden of non-communicable diseases in low-income countries.
The Question
Health screenings are an important tool to improve population health. In high and middle-income nations, blood pressure (BP) screening can reduce risk of cardiovascular disease, the leading cause of death and disability for adults 50 and older. However, population-based screenings remain limited in rural and low-income contexts.
In this study, the authors examined the sustained impact of BP screening for adults in rural Malawi, a low-income country in sub-Saharan Africa. Each participant had three BP measurements taken. Those with high BP received a letter referring them to a health care provider.
The Findings
Blood Pressure & Hypertension
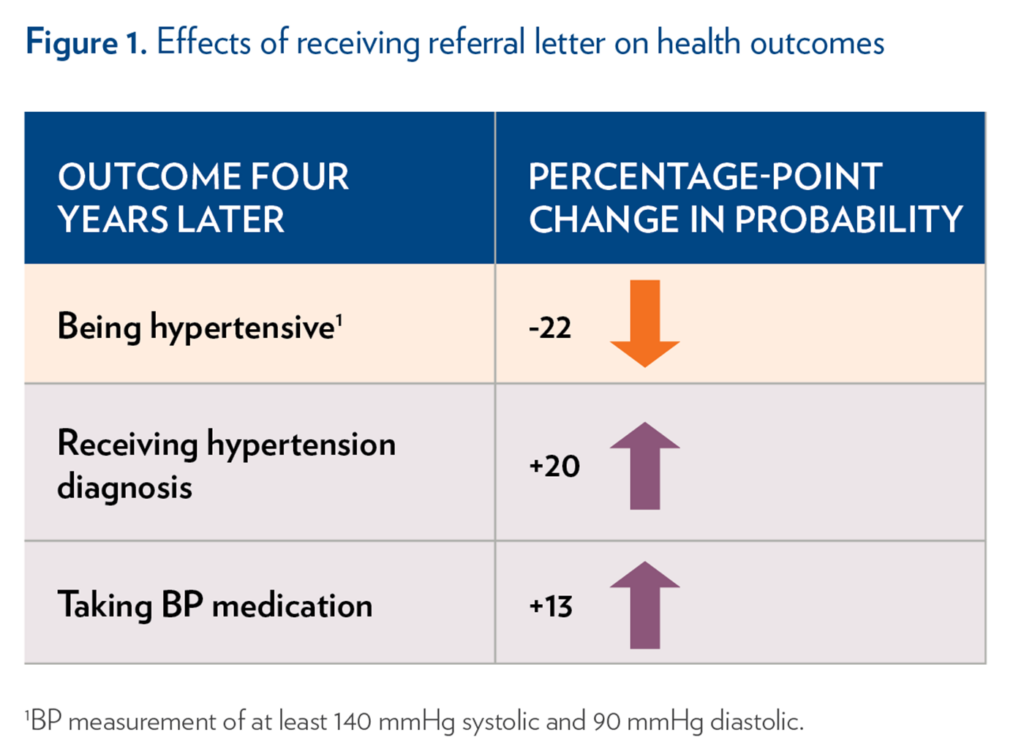
About 19% of adults in the study received a referral letter. At four- year follow-up, receiving a letter reduced the probability of beinghypertensive by 22 percentage points (Figure 1) and lowered both systolic and diastolic BP. Compared to similarly at-risk people who did not receive a letter, those who received a letter were 20-percentage points more likely to be diagnosed with hypertension after their screening and 13-percentage points more likely to be taking BP medication, suggesting that many saw a health care provider (Figure 1).
Health Knowledge, Behaviors, and Subjective Health
Receiving a referral letter did not affect participants’ knowledge of high BP treatments and symptoms. Further, it increased participants’ likelihood of engaging in certain unhealthy behaviors. At follow-up, participants who received a referral letter consumed, on average, 1 more teaspoon of sugar in their tea or coffee. They were also more likely to reduce their physical activity (by over 8 hours of vigorous physical activity per week) than their counterparts who did not receive a letter. However, there was no effect on the likelihood of adding extra salt to their plate or consuming sweet drinks. One possible explanation for this increase in certain unhealthy behaviors could be that some participants who received a letter may have substituted medication for exercise and diet change.
Notably, receiving a referral letter positively impacted participants’ mental health. At follow-up, those who received a letter were more likely to report favorable mental health than their counterparts who did not receive a letter. However, receiving a letter did not substantially affect participants’ assessments of their physical health or projected five-year survival.
The Implications
Among adults at risk of hypertension in rural Malawi, providing a simple referral letter effectively reduced BP and hypertension over four years. It also had positive effects in other health dimensions, including subjective mental health and probability of taking BP medication.
This is one of the first studies to document long-term health effects of a simple screening for non-communicable disease in sub-Saharan Africa. Overall, the findings suggest that while individuals are willing to spend time and effort to treat non-communicable disease, they are less willing to modify their habits and daily routines to prevent it. Importantly, rural, low-income populations may have different modifiable risk factors for disease than high or middle-income populations. Future research should examine the pathways through which participants in rural and low-income contexts achieve a reduction in BP and how this differs from other settings.
The Study
The authors analyzed data from the Mature Adults Cohort of the Malawi Longitudinal Study of Families and Health (MLSFH-MAC, 2012-2018), which includes adults ages 45+ in rural areas of three Malawi districts. All participants received a BP screening in 2013 and again in 2017, in which their diastolic and systolic BP was recorded three times. The study included 1,075 adults with an average age of 62 years. The survey also captured participants’ knowledge of hypertension-related health behaviors, treatments, diagnoses, and subjective health.
Participants were “at risk” for hypertension if they had at least one BP measurement above a threshold of 160 millimeters of mercury (mmHg) systolic and/or at least one measurement above 110 mmHg diastolic. At-risk participants received a short referral letter for further assessment by a nurse or doctor.
The authors used regression discontinuity and matching to evaluate the health effects of receiving a referral letter. First, they compared health outcomes of individuals with a maximum BP measurement right above the threshold (i.e., who received a letter) to those right below the threshold (i.e., who did not receive a letter, but had similar BP). Second, they calculated individuals’ “true” systolic BP by averaging participants’ three systolic BP measurements. They matched individuals based on their average BP at baseline (i.e., some of whom received a letter, and some of whom did not) and compared their health outcomes at follow-up. Both analyses controlled for sex, age, and regional variables.
Ciancio, A., Kämpfen, F., Kohler, H.-P. , and Kohler, I.V. (2021). Health Screening for Emerging Non-Communicable Disease Burdens Among the Global Poor: Evidence From Sub-Saharan Africa. Journal of Health Economics. doi: 10.1016/j.jhealeco.2020.102388. This brief is supported by the Penn Population Aging Research Center, funded by the National Institute on Aging (2P30AG012836-26).