
One Agency’s Maps Are Known For Documenting Redlining
But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says
Population Health
Blog Post

Co-posted with the Center for Pediatric Clinical Effectiveness (CPCE) at The Children’s Hospital of Philadelphia
Human papillomavirus (HPV) has devastating health impacts, causing over 30,000 cases of cancer and over 4,000 deaths each year in the United States alone. Despite a safe and effective HPV vaccine for adolescents, in 2019, only 54% of adolescents had been fully vaccinated, far from national goals of 80%. Clinician-based communications trainings are proven tools that can address vaccine hesitancy and increase HPV vaccine delivery.
Parental hesitancy has contributed to HPV vaccine refusal or delay, but clinician-focused decision support, including vaccine alerts and education, are tools that can increase HPV vaccine receipt in primary care. In addition, adolescents who receive a strong provider recommendation are more likely to receive the HPV vaccine.
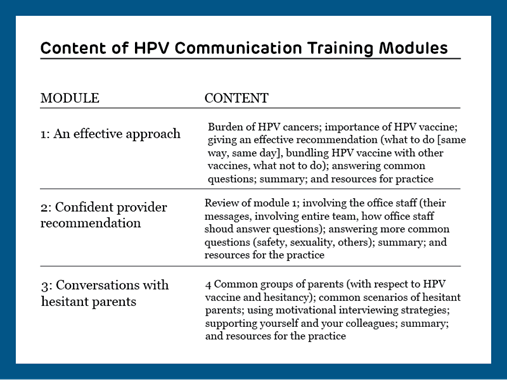
In-person communication training for clinicians has improved HPV vaccination rates in prior studies, but this training is difficult to provide on a large scale. To broaden its impact, our team developed and tested an online communication training, designed to improve how clinicians communicate with parents about HPV vaccines within pediatric primary care settings. Throughout the study, clinicians completed online modules and received weekly ‘Quick Tips’ via text message and email. Modules described the problem of HPV, how to give an effective HPV recommendation, how to answer common questions, and how to engage office staff. Quick tips reinforced the content from each of the modules.
We used electronic health record (EHR) data from 48 pediatric primary care practices to evaluate missed opportunities for vaccinations, defined as a visit at which HPV vaccine was due but not administered. Separately, we looked at missed opportunities for initial and subsequent vaccine doses at well child care (WCC) visits and acute or chronic visits during an initial 12-month baseline period, and during the 6-month intervention period.
We found that missed opportunities decreased more in intervention practices than in control practices from baseline to the intervention period overall (2.4 percentage points), at initial WCC visits (6.8 percentage points) and at subsequent WCC visits (2.5 percentage points). Missed opportunities did not change at acute or chronic visits, which are less common settings for a vaccine conversation than well-child visits.
Most adolescents who initiate the HPV vaccine series go on to receive subsequent doses, so the impact of the communication intervention on vaccine initiation is promising. Given the prevalence of vaccine hesitancy within pediatric care, and the national focus on COVID-19 vaccinations, enhanced provider communication is integral to ensuring higher rates of vaccine delivery. Our results suggest that clinicians who learn and use the communication approaches tested can more effectively vaccinate teens and prevent a common cancer.
Multicomponent interventions like feedback reports and EHR-generated prompts, used in combination with communication skills training, could decrease missed opportunities even further. Testing of these approaches in combination is warranted.



But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says

Offit and Buttenheim Criticize HHS Placebo Trial Mandate as Unethical, Misleading, and a Threat to Vaccine Confidence

A Penn LDI Virtual Seminar Explores the Latest Trends in Anchor Institution Operations

Neighborhood Perceptions May Also Affect PTSD and Depression Recovery After Serious Injury

A Penn LDI and Opportunity for Health Lab Virtual Seminar Explores Economic Assistance Programs

Testimony: Delivered to Philadelphia City Council