
One Agency’s Maps Are Known For Documenting Redlining
But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says
Population Health
Blog Post
The way we measure birth complications during a hospital stay is incomplete and needs to be changed, according to a new study from LDI Associate Fellow Sara Handley and Senior Fellow Scott Lorch.
In response to alarmingly high U.S. infant and birth parent mortality, the Biden administration is launching efforts to promote safer childbirth, which requires reliable measures to track progress.
Handley and coauthors developed a measure of childbirth complications during hospitalization that improves on current measures by using data on both the newborn and parent, instead of one or the other. The approach makes sense because their risks and outcomes are linked: For example, there is an increased parental infection risk when neonatal distress leads to a cesarean delivery.
Handley and colleagues used birth, death, and hospital discharge data from 2010-18 on more than 6.6 million infant-parent pairs from California, Michigan, Oregon, Pennsylvania, and South Carolina. They developed measures of complications and severe complications for childbirth hospitalization that included deaths, intensive care admissions, or infections.
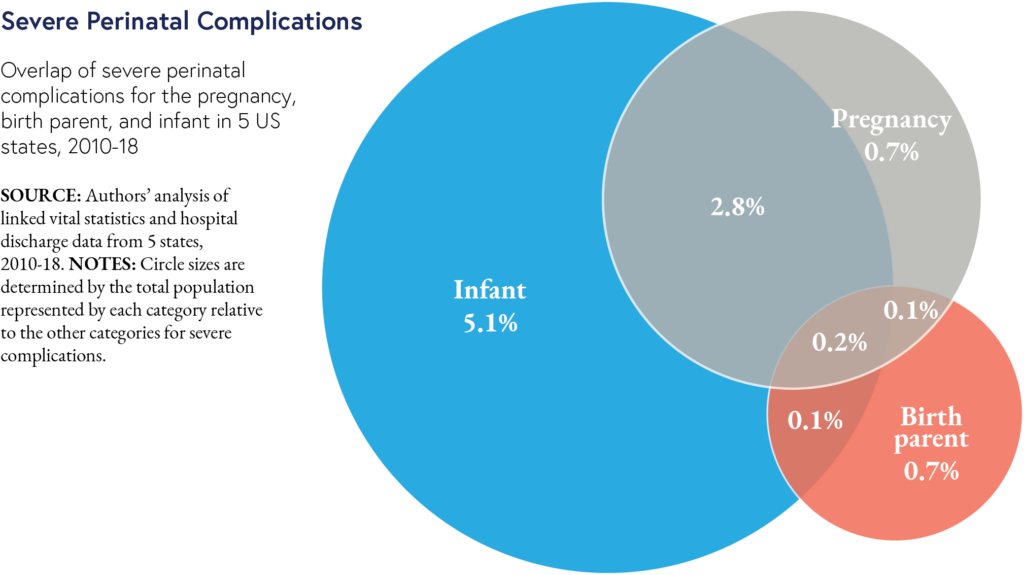
The new measures showed that nearly 10% of births had severe complications. When complications were categorized by birth parent-only, infant-only, or pregnancy, overlap was low. In the figure for severe complications, only 0.2% of patient-infant pairs had complications that would be picked up by measuring only one category—so reporting only a single measure of childbirth complications misses many adverse events.
An advantage of the new measure is its focus on birth hospitalization, when improvement actions are feasible. Hospitals can design quality improvement initiatives and interventions for events that occur when both parent and child are under their care.
The new measure supports the Biden administration’s Blueprint for Addressing the Maternal Health Crisis and the Centers for Medicare and Medicaid Services’ “Birthing-Friendly” hospital designation based on care quality and safety. The country’s major health plans are committed to using this designation. The impact of these initiatives could be greater by using comprehensive metrics of care such as the measure of childbirth care proposed by Handley and colleagues.
The study, “Perinatal Care Measures Are Incomplete If They Do Not Assess The Birth Parent-Infant Dyad As A Whole,” was published in September 2023 in Health Affairs. Authors include Sara C. Handley, Brielle Formanowski, Molly Passarella, Katy B. Kozhimannil, Stephanie A. Leonard, Elliott K. Main, Ciaran S. Phibbs, and Scott A. Lorch.


But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says

Offit and Buttenheim Criticize HHS Placebo Trial Mandate as Unethical, Misleading, and a Threat to Vaccine Confidence

A Penn LDI Virtual Seminar Explores the Latest Trends in Anchor Institution Operations

Neighborhood Perceptions May Also Affect PTSD and Depression Recovery After Serious Injury

A Penn LDI and Opportunity for Health Lab Virtual Seminar Explores Economic Assistance Programs

Testimony: Delivered to Philadelphia City Council