
HIV is Not a Crime: The Case for Ending HIV Criminalization
Outdated Laws Target Black and Queer Lives in Over 30 States, Fueling a Deadly Disease
Blog Post
How can we make the best use of scarce donor organs? This is a constant question for those of us involved in the care of patients with liver disease. Patients are prioritized for transplant following a “sickest first” principle, but what if the current system underestimates the degree of “sickness” for an entire class of patients? This issue is at the heart of a debate surrounding acute on chronic liver failure (ACLF), a recently-established syndrome that carries high short-term mortality —over 50% through 90 days.
Calls to change organ allocation policies for patients with ACLF follow research studies demonstrating higher than expected waiting list mortality among ACLF patients. However, these studies are largely based on data from the national transplant registry (the United Network for Organ Sharing [UNOS]), which lacks key variables that are needed to properly classify ACLF. To better understand the accuracy of UNOS ACLF classifications, my colleagues and I performed a multicenter study comparing them to ACLF diagnoses and severity grades derived from manual chart review.
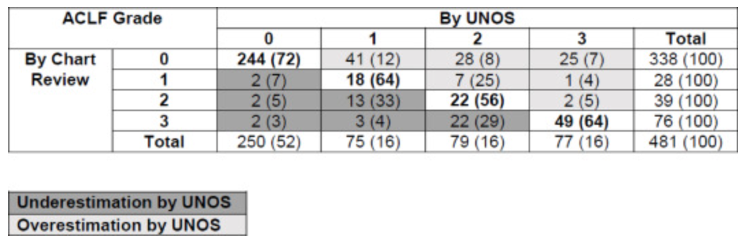
As we reported in the Journal of Hepatology, we reviewed the charts of 481 patients across three health systems and found that the agreement between UNOS-classified ACLF and manually verified ACLF was only 64% for severe (grade 3) ACLF. Furthermore, across different ACLF severity grades, the UNOS classification approach frequently underestimated and overestimated ACLF severity. More concerning, 27% of patients who did not have ACLF (grade 0) were incorrectly classified as having ACLF using the UNOS classification approach.
There are several important lessons learned from our study. The UNOS data collection process could be improved to better capture ACLF by modifying and adding to the list of data that is collected for patients listed for transplant. For example, in our review, we found that adding information about acute exacerbations of disease would be beneficial to help properly classify patients. This will be critical for both future ACLF research and for the identification of patients with ACLF if future changes lead to increased priority. More broadly, when considering the economics of transplantation and organ scarcity, prioritization of one group disadvantages another. To make the best use of organs donated for transplant, we must ensure the validity of the UNOS classification system for all medical conditions, even those that are newly identified. Manual chart review may inform improvements to the UNOS system so that patients who could benefit the most from organ transplantation are properly identified and prioritized.
The study, Discordance in Categorization of Acute-on-Chronic Liver Failure in the United Network for Organ Sharing Database, was published in the Journal of Hepatology, January 21, 2022 by Brian P. Lee, Giuseppe Cullaro, Aidan Vosooghi, Frederick Yao, Sarjukumar Panchal, David S. Goldberg, Norah A. Terrault, and Nadim Mahmud.


Outdated Laws Target Black and Queer Lives in Over 30 States, Fueling a Deadly Disease

Selected for Current and Future Research in the Science of Amputee Care

Penn LDI Seminar Details How Administrative Barriers, Subsidy Rollbacks, and Work Requirements Will Block Life-Saving Care

Top Experts Warn of Devastating Impact on Community Safety Efforts

A Gathering of a Health Services Research Community Currently Under Siege

1,000+ Detail the Latest Health Services Research Findings and Insights

Wharton and LDI’s Joanne Levy Takes the Stage at AcademyHealth

New Penn LDI Study Is Based on Hospital Incident Reports Rather Than Electronic Health Records