Health Equity
Blog Post
Maternal Resilience and Low Birthweight
Resilience Helps, Disparities Remain
The United States has one of the highest rates of low birthweight (LBW) among OECD countries, with significant disparities by race and ethnicity. We know that maternal “resilience”—protective factors that buffer the health effects of stress and adversity—may be associated with lower LBW rates, but the relationship among maternal resilience, race/ethnicity, and LBW is not clear. Identifying resilience and LBW patterns by race/ethnicity is important to target prevention efforts.
In a study in the Journal of Perinatology, Diana Montoya-Williams, Scott Lorch, and colleagues found substantial racial/ethnic differences in maternal resilience, which was associated with LBW rates. Women with higher resilience were less likely to deliver a LBW infant, but resilience was not able to overcome racial/ethnic LBW disparities.
The authors studied 3,244 women who self-reported as non-Hispanic (NH) white (66.5%), non-Hispanic Black (15.2%), American Indian (AI) (2.4%), Asian (2.9%), Hispanic (12%), and other (1%). In this national cohort, 13.5% of all births were LBW (infants weighed <2500 grams). NH Black women had the highest rate of low birthweight (20.1%), nearly twice that of their NH white counterparts (11.4%).
Using a validated instrument, the authors assigned each participant a resilience score (maximum of 29, with higher scores indicating more resilience). The median resilience score for the cohort was 14, with significant differences by race/ethnicity. Overall, AI and Asian participants had the lowest resilience scores of all racial/ethnic groups.
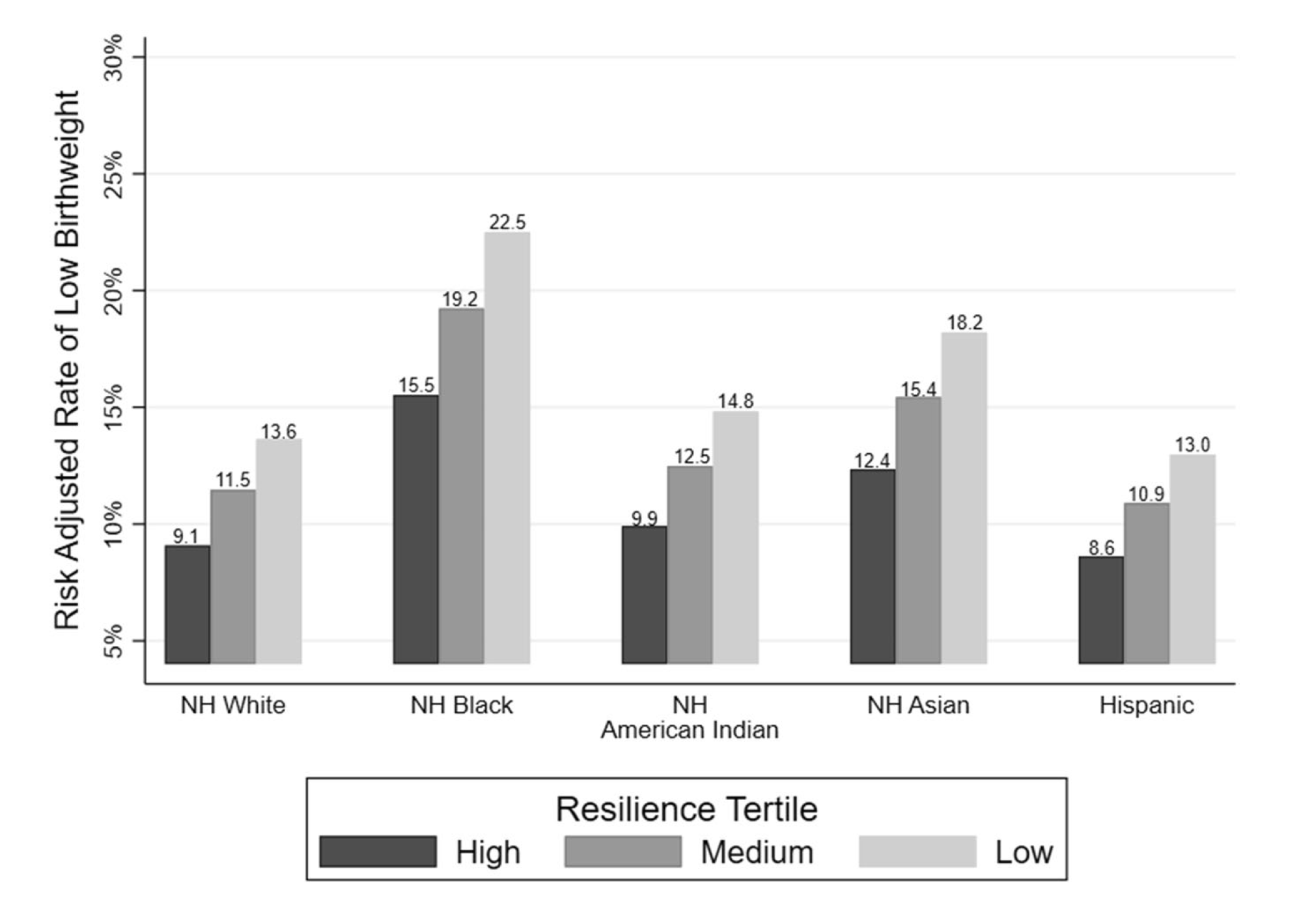
Mothers with high resilience (scores 20-29) were 1.6 times less likely to deliver a LBW infant than mothers with low resilience (scores <10). However, the protective effect of maternal resilience did not transcend baseline racial differences in LBW risk. After adjusting for maternal age, education, household income, and other factors, highly resilient NH Black women still had higher rates of LBW than highly resilient NH white and Hispanic women (Figure 1). Similarly, NH Black women with the lowest resilience scores had a significantly higher LBW rate (22.5%) than NH white women (13.6%) and Hispanic women (13.0%) with comparable resilience.
Beyond the neonatal period, LBW has negative long-term health consequences. These findings suggest that differences in maternal resilience do not entirely account for racial/ethnic disparities in LBW. Given the high rate of LBW among highly resilient NH Black participants, the authors raise questions about whether the impact of stress on birthweight is particularly magnified in these women.
Since race is a social construct that could be measuring the impacts of racism, the authors acknowledge that this study’s focus on individual resilience cannot fully account for LBW disparities among NH Black participants. Future research examining the relationship between resilience and birthweight should also examine the structural roots of racism that trigger stress among NH Black mothers. Research recognizing racism and its effects—studies that include patient perspectives and focus on relationship-centered care—could inform more effective LBW prevention efforts.
The study, Racial/Ethnic Differences in Maternal Resilience and Associations With Low Birthweight, was published in the Journal of Perinatology Society in October 2020. Authors include Diana Montoya-Williams, Molly Passarella, William A. Grobman, and Scott A. Lorch.