Improving Care for Older Adults
Brief
Patient Outcomes After Hospital Discharge to Home with Home Health Care vs to a Skilled Nursing Facility
Home health care leads to savings despite increasing hospital readmissions

JAMA Internal Medicine – published March 11, 2019
KEY FINDINGS
In this study of more than 17 million Medicare hospitalizations between 2010 and 2016, patients discharged to home health care had a 5.6 percent higher 30-day readmission rate than similar patients discharged to a skilled nursing facility (SNF). There was no difference in mortality or functional outcomes between the two groups, but home health care was associated with an average savings of $4,514 in total Medicare payments in the 60 days after the first hospital admission.
THE QUESTION
Medicare is the largest payer of postacute care, spending more than $60 billion on it in 2015 alone. More than 40% of hospitalized Medicare patients receive postacute services after discharge, mostly in the home or in a skilled nursing facility. However, it is unclear whether the choice of postacute care setting affects patient outcomes and costs. Understanding the tradeoffs between postacute care settings is particularly important as alternative payment models push patients to lower-cost settings for postacute care. The authors investigated differences in rates of 30-day readmission, 30-day mortality, functional outcomes, and Medicare payment for a very large national sample of Medicare beneficiaries (including traditional Medicare and Medicare Advantage patients) discharged to home health care versus an SNF, using a rigorous methodology to control for confounding factors.
THE FINDINGS
Between 2010 and 2016, more than 17 million Medicare beneficiaries were discharged to postacute care: 39% to home health and 61% to an SNF. Patients discharged to home health care had a 5.6% higher readmission rate at 30 days than those discharged to an SNF. The difference was driven by readmissions that were potentially discretionary, rather than those for which hospital treatment is nearly always advised (e.g., respiratory failure). The two groups did not differ in terms of improved functional status during postacute care nor in 30-day mortality.
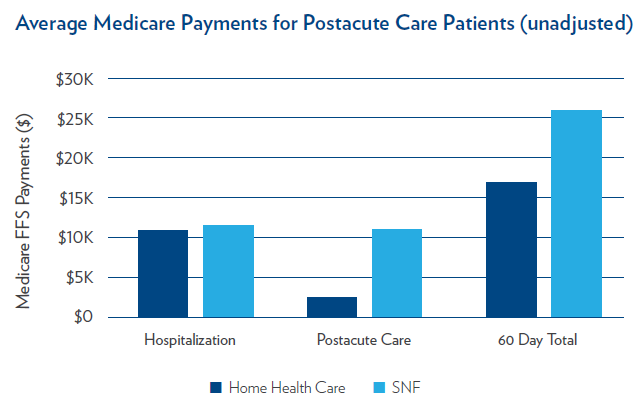
Medicare fee-for-service payments for the initial hospitalization, postacute care, and the total payment in the first 60 days after admission for both groups are shown in the figure below. After adjusting for confounding factors, postacute care was significantly lower for those discharged to home health (an average savings of $5,385 per beneficiary), as was the total Medicare payment within the first 60 days following hospital admission, with average savings of $4,514 per beneficiary. It is notable that home health care was associated with this level of savings despite a significantly higher hospital readmission rate.
THE IMPLICATIONS
This study provides the first large scale and recent estimates of the differences in patient outcomes and Medicare spending between home health care and SNFs. There are several reasons why discharge to SNFs may prevent readmissions. SNFs are able to provide 24-hour monitoring of patients, which may help prevent complications that could lead to unnecessary hospital readmissions. SNFs are also able to provide a higher level of treatment intensity compared to care received in the home. This level of care comes with a cost, however, as institutional postacute care is associated with higher Medicare payments than home health care. Further research may be helpful to better understand the profiles of beneficiaries that would most benefit from SNF care or who are least likely to be readmitted after discharge to home health care.
Payment reform implemented after the passage of the Affordable Care Act has driven hospitals to reduce readmissions at the same time as alternative payment models have incentivized lowering costs. Optimal clinical decisions will involve balancing these incentives. While this study found that SNFs were associated with reduced readmissions compared to home health care, they were associated with increased Medicare spending. Policymakers and clinicians should consider how best to draw on the benefits of both settings to increase the value of postacute care.
THE STUDY
The authors use data from Medicare beneficiaries who were discharged from hospital to home health care or an SNF between January 1, 2010 and December 31, 2016. Data included U.S. short-term acute-care hospital Medicare claims, and reports from SNFs and home health assessments. Unlike previous research on this topic, this study uses a large dataset of over 17 million hospitalizations, controls for differences in patient characteristics across care settings, and includes patients with many different conditions.
While patients were not randomly referred to an SNF vs home health care, the authors’ methodology creates a comparable dataset, controlling for factors that may have influenced choice of postacute care setting. The adjusted outcomes of this study apply to patients referred to home health care who could have reasonable been referred to an SNF instead. The characteristics of these patients are similar to those of the average Medicare beneficiary in the study, increasing the generalizability and importance of results.
LEAD AUTHOR

Rachel Werner, MD, PhD is a Professor of Medicine, Director of Health Policy and Outcomes Research in the University of Pennsylvania’s Department of Medicine and Associate Chief for Research in the Division of General Internal Medicine. Over the past 15 years, Dr. Werner has built a foundational research program examining the effects of health care policies on health care delivery, using methods designed to draw causal inference from observational data. She divides her time between research on quality of care and her primary care practice at the Philadelphia VA and also co-directs Penn’s Master of Science in Health Policy Research.
Her study co-authors are Norma Coe, PhD, Associate Professor of Health Policy at the Perelman School of Medicine at the University of Pennsylvania, Mingyu Qi, MS, statistical analyst with the Health Economics Data Analyst Pool at the University of Pennsylvania, and R. Tamara Konetzka, PhD, Professor in Health Services Research in the Department of Public Health Sciences at the University of Chicago.