Improving Care for Older Adults
News
Penn Nursing School/LDI Research Team Wins NAM Catalyst Grant Award
Sense4Safety Project Added to Global Innovation Tournament for Improving Elder Care

A University of Pennsylvania research team headed by three School of Nursing Professors and LDI Senior Fellows has won a National Academy of Medicine (NAM) Healthy Longevity Global Grand Challenge Catalyst Award supporting work on “Smart Home” monitoring technologies for socially vulnerable elders. Called Sense4Safety, the project by George Demiris, PhD, FACMI; Therese Richmond, PhD, RN, FAAN; and Nancy Hodgson, PhD, RN, FAAN, uses passive monitoring systems installed as part of a nursing intervention in the homes of frail older adults in low-resource neighborhoods.
“Sense4Safety is a nursing-driven intervention designed to prevent falls,” said Richmond, who is Associate Dean of Research & Innovation at the School of Nursing, and Research Director of the Penn Injury Science Center (PISC). “We’re capitalizing on what Penn does best — integrating knowledge — as we bring together passive remote sensing, artificial intelligence, nursing and engineering expertise in working with at-risk, vulnerable populations.”
The Penn Sense4Safety project is one of 124 that received a Catalyst Award in the first round of NAM’s new program.
Founded by NAM and launched in December of 2019 in collaboration with the National Institute on Aging (NIH), the Healthy Longevity Global Grand Challenge is essentially a global innovation tournament designed to accelerate scientific advances related to health care and the elderly.
Urgent research need
The NAM website explains, “At the current pace, population aging is poised to impose a significant strain on economies, health systems, and social structures worldwide. Multidisciplinary solutions are urgently needed to maximize the number of years lived in good health and a state of well-being.”
In his video introduction to the program, NAM President Victor Dzau, MD, says, “We are at an inflection point that says to us if we can do the right thing, we can make huge differences. The mission of the National Academy of Medicine is to accelerate the progress of science, medicine, health and policy. We have always been in the forefront addressing the issue and that’s why we are so excited about taking on longevity and aging. It is the grand challenge of our time.”
The third and final phase will be a $5 million grand prize to the research team that has achieved ‘a breakthrough innovation that extends the human health span.’
NAM competition
The first phase of the three-year program will provide seed funding to 450 research projects. The second phase will provide $500,000 each to two select finalists. The third and final phase will be a $5 million grand prize to the research team that has achieved “a breakthrough innovation that extends the human health span.”
The first round of phase one Catalyst awards went to research teams in the US, UK, European Union, Israel, Singapore, Japan, Taiwan and Tanzania. Two University of Pennsylvania teams were selected for Catalyst awards.
Keen focus on remote monitoring
It’s interesting to note that 33, or 27 percent of this first round of Catalyst award projects, involve AI-augmented devices that facilitate some kind of continuous remote monitoring of vulnerable elderly in their homes. These range from smart toilet seats that monitor vital signs and smart socks that measure muscle functions, to smart inflatables that prevent fall-related hip fractures and disposable smart patches that detect early signs of infectious disease.
There is also a bevy of smartwrist- and smartphone-connected apps — to measure functional decline, detect pathogens in saliva, calculate fall risk, remotely supervise elder exercise, monitor blood vessel stiffening, and deliver wheelchair maintenance reminders.
The Smart Home idea, used by Penn’s Sense4Safety project, is based on the already established “Internet of Things” concept (IoT). In IoT, a home’s kitchen appliances, washers and dryers, HVAC functions, locks, lighting, blinds, media devices, security systems, and internal web security cameras are interactively connected via a network hub that controls the components and gathers data about their use and maintenance. In the current commercial versions, these network-of-things installations are also tethered to family members’ smartphones.
Behavior sensing devices
The elder health care-related version of this wires up a house or apartment in a similar manner. Various behavior-sensing devices are connected to the network that collects and feeds constant streams of data to a cloud-based server for analysis. That server, in turn, feeds back charts and graphs to a computer dashboard made available to either the patient or designated family members or both. It can also feed any aspect of its data to relevant clinician offices.
Smart home technology is a burgeoning new industry; current commercially available devices include:
• Motion sensors that document the occupant’s movements and provide data on things like whether the patient is or becomes sedentary, or the number of bathroom visits made during the night.
• Appliance-specific motion detectors for things like refrigerators
• Door and window sensors that document how much time is spent in or out of the home, as well as how many visitors a patient may or may not have.
• Intelligent stove sensors that distinguish between routine meal preparation versus forgetfully leaving the burners on.
• Temperature and luminosity sensors.
• Web cameras designed to facilitate online web video communications with clinicians and family (but not surveil the patient’s daily activities).
• Voice-operated smart speakers, like health-centric “Alexa” systems facilitating quick and easy access to basic health care information.
This last is also designed to provide voice control capabilities to elders with disabilities who can use the hub to remotely voice control door locks, light switches, window blinds, and other household devices.
Unique Penn team perspective
While some of these individual technologies have previously been used in health care venues, the Penn team’s research is the first to evaluate health care-oriented in-home networks of devices centrally controlled from a cloud server.

In late November, Richmond and Demiris participated in the “Smart Beds, Homes and Robots: Emerging Tech Opportunities for Aging” webinar co-sponsored by the School of Nursing and the Penn Roybal Center on Palliative Care in Dementia. Richmond moderated the event and Demiris’ panel presentation was an explanation of the Sense4Safety project focused on it’s most unique new component: the depth sensor.
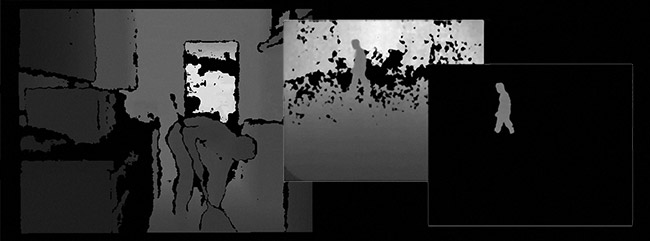
Designed to be mounted high on the wall overlooking a room, depth sensors are infra-red video cameras and processing devices that record black and white silhouette images and calculate the exact depth — or distance from the camera lens — of every point in the image. Over time, they can document subtle patterns of motion. For instance, they can detect when a person’s gait — or slight variations in limb movements in relation to each other — might change. Such a change can have major health implications for frail elders.
‘Reading’ gait characteristics
Demiris explained that research colleagues at the University of Missouri have developed a system to extract data about gait characteristics from depth sensor feeds. It’s very useful in calculating fall risk. They’ve found that a cumulative decrease of 5.1 cm per second over seven days in in-home gait is associated with an 86.3% probability of falling within the coming three weeks, compared with a 19.5% probability for those with no gait change.
“Falls are one of the highest level challenges older adults face when trying to remain independent in the community,” said Demiris. “Accumulated vulnerabilities and mild cognitive impairment or housing conditions are independent risk factors for falls. Over 60% of older adults with mild cognitive impairment fall annually; that’s two to three times the rate of those without cognitive impairment. Additionally, older adults living in low resource neighborhoods with poor housing conditions have twice the rates of falling.”
“The Sense4Safety work,” Demiris continued, “is a technology-supported intervention that aims to identify escalating risk for falls in real time through in-home passive sensor monitoring, and then use machine learning to inform the digitalized plans to reduce that fall risk for any given individual.”