Blog Post
Predicting Surgical Risk in Patients with Cirrhosis
New Tool Improves Predictions
Patients with cirrhosis have a high risk of post-operative mortality. As the burden of cirrhosis continues to rise in the United States, it is critical to ensure that we are properly assessing this risk for vulnerable patients prior to surgery. There are concerns in the hepatology and surgical communities that existing prediction tools tend to overestimate the risk, resulting in many patients being denied surgeries that might otherwise be safe to perform.

In a recent study in Hepatology, my colleagues and I developed and tested a novel risk prediction tool—the VOCAL-Penn score—to provide more accurate post-operative mortality predictions for patients with cirrhosis. Using national data of nearly 4,000 veterans with cirrhosis who underwent major surgeries, we compared the VOCAL-Penn Score to three existing tools: the model for end-stage liver disease (MELD), Child-Turcotte-Pugh (CTP), and the Mayo risk score.
First, we found that the Mayo risk score did in fact overestimate surgical risk in patients across the entire surgical risk spectrum. Next, in evaluating the performance of the VOCAL-Penn score, we found that it was much more accurate in predicting surgical risk at multiple post-operative timepoints. For example, in an aggregate measure of performance (the area under the receiver operating characteristic curve, or AUROC), VOCAL-Penn had an 87% chance of distinguishing patients who died from those who did not at 30 days after surgery, compared to 77% for the Mayo risk score and 72% chance for MELD.
These findings have important clinical implications, as historically high perceptions of cirrhosis surgical risk have resulted in avoidance of surgery for many patients, even when the risk of surgery would be acceptable in reality. This is especially important for patients who are denied elective surgery until the indication becomes emergent, where the surgical risk is universally higher (e.g., for an abdominal hernia that later becomes incarcerated).
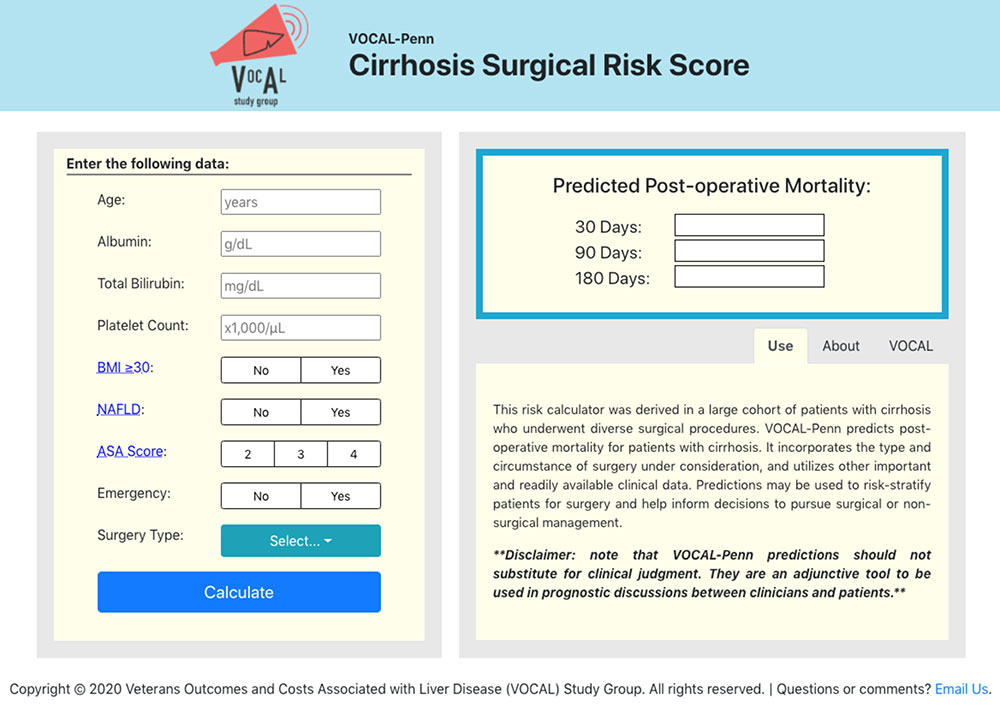
How did we improve upon existing tools? Recognizing that most models focused almost exclusively on the severity of liver disease, we incorporated both the type of surgery and the urgency of the indication (i.e., emergency or routine) in our tool. We also used modern inferential methods to more precisely model the impact of important clinical indicators on mortality, such as laboratory predictors and comorbidities. We specifically included non-alcoholic fatty liver disease and obesity, which have become increasingly salient in determining post-operative outcomes for patients with cirrhosis.
Pending external validation studies, which are ongoing, clinical uptake of the VOCAL-Penn risk calculator may serve to shift perceptions of cirrhosis surgical risk to better match the reality of the current landscape. Beyond validating the model, it may also help us evaluate potential interventions to mitigate post-operative mortality risk, such as placement of a transjugular intrahepatic portosystemic shunt (TIPS), use of non-selective beta blockers, and nutritional optimization. The VOCAL-Penn risk calculator can be found at www.vocalpennscore.com.
The study, Novel Risk Prediction Models for Post‐Operative Mortality in Patients with Cirrhosis, was published online in Hepatology on September 16, 2020. Authors include Nadim Mahmud, Zachary Fricker, Rebecca A. Hubbard, George N. Ioannou, James D. Lewis, Tamar H. Taddei, Kenneth D. Rothstein, Marina Serper, David S. Goldberg, and David E. Kaplan.