
Meaningful Representation in Clinical Trials Strengthens Science
Failure to Include Diverse Populations Undermines Innovation in the Age of Precision Medicine
Blog Post
As the nation continues to grapple with outbreaks of COVID-19, the Biden Administration released a statement that concludes a booster shot will be needed to maximize vaccine-induced protection. So, the question remains: How should these boosters and attendant resources be allocated, so that communities that are most vulnerable and disadvantaged are prioritized?
Throughout the pandemic, Black and Brown people have overwhelmingly borne the brunt of disease incidence and mortality. In response, many jurisdictions have used various forms of place-based “disadvantage indices” in their initial vaccine rollouts to identify and target vulnerable communities. These initial experiences may be instructive in the allocation decisions we will once again be facing as a nation.
In a recent study in Nature Medicine, Harald Schmidt and colleagues analyzed the vaccine allocation plans of 64 U.S. jurisdictions (50 states, DC, eight territories, and five large cities), to describe whether and how they used disadvantage indices within and across vulnerable groups. They found that the majority of states (n=34) used a disadvantage index, and nearly half of them explicitly aimed to advance equity within allocation phases. Jurisdictions used these indices in a variety of ways, including:
Since that study was conducted, a new type of disadvantage index was launched earlier this month by the Centers for Disease Control and Prevention (CDC) and the Office of Minority Health at the U.S. Department of Health and Human Services (HHS): the Minority Health Social Vulnerability Index (SVI), uses U.S. Census data to geographically identify “racial and ethnic minority communities at greatest risk for disproportionate impact and adverse outcomes due to the COVID-19 pandemic.”
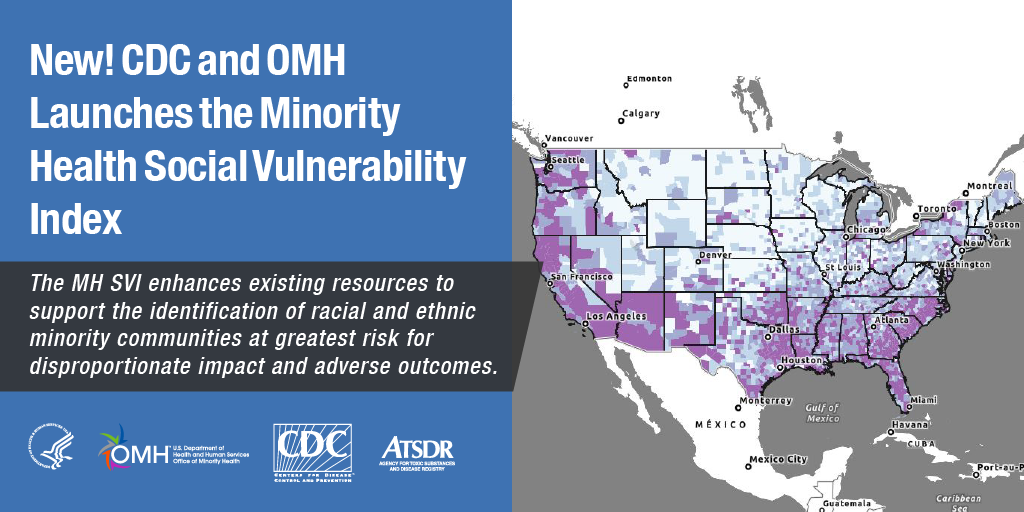
The Minority Health SVI builds upon the CDC’s previous SVI, which used 15 social risk factors, by adding COVID-19 relevant data themes such as “Health Care Infrastructure & Access” and “Medical Vulnerability”. Additionally, the newer index lists specific race/ethnicity categories and languages to provide more precise data. The Minority Health SVI can be applied in various ways, from research to program design to strategic planning. It is available as a user-friendly “Data Dashboard” that allows the user to select variables, define geographic areas, filter by overall vulnerability or specific themes, and map the results.
Schmidt and colleagues point out that the widespread use of disadvantage indices during COVID-19 holds considerable potential to promote health equity, especially when matched with vigorous strategic planning to provide the vaccine in trusted community environments. In ongoing survey research, Schmidt found that 51% of Americans support the use of disadvantage indices as implemented, and just 16% oppose them. In remarks to the White House Health Equity Task Force this month, Schmidt noted this support and the importance of these indices as the pandemic continues and booster shots are considered:
[T]he pandemic is, unfortunately, of course not over yet, and there is an active discussion about booster vaccines…clearly, the question of boosters has to be driven by science. And ideally, given the unbearable global vaccine access disparities, we would only roll out boosters if this does not compete with closing the unacceptable global vaccination gap. But if and when there is a reasonable case for boosters, initially, there will again be severe scarcity if not even a marginally different type of vaccine should be used, and if the same type should be used, the question also arises as to which population groups should be offered them first.
Pending FDA approval, it appears that booster shots will be available in the U.S. in late September. If and when they are, the lessons learned in the initial rollout, and the new tools available to identify and target vulnerable communities, could have profound implications for equity and public health.


Failure to Include Diverse Populations Undermines Innovation in the Age of Precision Medicine

A Wharton–Netter Center Collaboration Uses Experiential Learning to Build a Health Care Workforce Pipeline

The Odd Paradox of the Big Beautiful Bill’s Health Care Goals

Lower Pay for Black and Hispanic Patients Drives Unequal Access to Care

Penn LDI’s Antonia Villarruel and 10 Other Authors Map Social Determinants Across Multiple Racial and Ethnic Groups

A New Study of a Sample of Facilities Found Half Without Any Behavioral Health Staff