Substance Use Disorder
Blog Post
Substituting Heroin for Prescription Opioids
An unintended consequence of well-intentioned policy
It seems self-evident: one way to address the epidemic of opioid deaths is to make prescription opioids harder to misuse. OxyContin, for example, is especially dangerous when it is crushed for ingestion, inhalation, or injection. In 2010, the FDA approved a reformulated, abuse-deterrent version of OxyContin that made the pill difficult to crush or dissolve. The new version immediately replaced the old one, marking a substantial reduction in the supply of abusable prescription pain relievers.
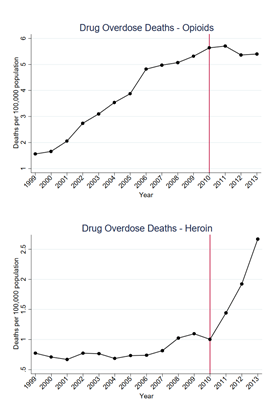
But policies have intended as well as unintended consequences, and one potential effect of the OxyContin reformulation could be substitution toward other opioids, such as heroin. A new study by Abby Alpert, David Powell, and Rosalie Liccardo Pacula, published as an NBER working paper, suggests that in the short-term, this is exactly what happened: reformulation did not decrease overall overdose deaths, because heroin deaths increased as OxyContin deaths decreased. These deaths largely offset each other.
These findings are consistent with national trends. After remaining relatively constant for several years, heroin-related overdose deaths quadrupled between 2010 and 2015. While the timing of this uptick suggests a link with the OxyContin reformulation, other policies were implemented around the same time. Some states adopted prescription drug monitoring programs (PDMPs), some opioids were taken off the market, and many Florida “pill mills” were shut down. Some research has suggested a causal relationship between reformulation and the rise in heroin overdoses based on these national trends, but a recent review article cast doubt on the connection.
The new study delves further to identify a causal substitution effect. The authors analyzed changes in death rates involving opioids over time and across states. They found that states with the highest initial rates of OxyContin misuse experienced the largest increases in heroin deaths, a differential that began precisely in the year following reformulation.
Moreover, heroin deaths were uncorrelated with OxyContin misuse prior to the reformulation: both the levels and trends in heroin deaths were nearly identical across states with high or low initial rates of OxyContin misuse before 2010. Further, they found that nonmedical use of OxyContin, specifically, predicts growth in heroin mortality while initial nonmedical use of pain relievers more generally does not. Since most policies— other than OxyContin reformulation— address opioids more broadly, this evidence is consistent with a causal impact of the reformulation. These results imply that the reformulation was associated with as much as 80% of the increase in heroin deaths.
The authors considered other reasons for the pattern in heroin deaths and ruled out state-level adoption of PDMPs. The Florida pill mills affected Florida as well as states such as Kentucky and West Virginia, but excluding these states did not affect the relationship between OxyContin misuse rates and changes in heroin mortality rates.
Does that mean that the FDA should abandon its efforts around abuse-deterrent prescription opioids? While the reformulation may lead to substitution across drugs for existing users (mitigating its effectiveness in the short run), the policy could also deter new abuse, which would broaden its effectiveness over time. In addition, the policy could have other beneficial effects that are not measured by short-term death rates.
As the FDA encourages the development of more abuse-deterrent opioids, it is important to consider the ramifications of this type of policy. The results suggest that supply-side policies may have unintended consequences when close substitutes are available. Broader and more comprehensive supply-side interventions may be more effective. Treating underlying demand through substance abuse treatment may also prove to be more effective for addressing existing users, particularly because substitutes are readily available.
While the study found detrimental effects in the short term, the overall effectiveness of abuse-deterrent formulations will become more evident over time as we observe whether reductions in new initiation eventually offset short-term substitution to heroin.
