Health Care Access & Coverage
Brief
The Future of Value-Based Payment: A Road Map to 2030
White Paper
Executive Summary
A decade after the passage of the Affordable Care Act, the vision of moving the U.S. health care system “from volume to value” has been partially realized, with few value-based payment initiatives systematically reducing spending or improving quality. While participation in value-based payments continues to grow, the adoption of advanced forms of value-based payment through alternative payment models lags behind both the goals set by the Secretary of Health and Human Services in 2015 and the threshold required for widespread practice transformation. Furthermore, the complexity of the current suite of alternative payment models and allure of traditional fee-for-service prevent the widespread adoption of full risk-bearing contracts. The high costs of care with the impending insolvency of the Medicare trust fund, persistence of poor quality of care and health disparities along racial and socioeconomic lines, and mixed success of alternative payment models indicate the need for a revamped vision for the 2020s.
The 2020s require a new strategy that moves from a short-term focus on testing new payment models to a long-term focus on expanding models that are most likely to generate substantial savings and improve quality. This white paper outlines a new direction for the federal government—primarily through the Centers for Medicare and Medicaid Services (CMS)—to chart over the next decade aimed at completing the transition to a health care system that pays for value and reduced health disparities, rather than high volumes of services.
First, CMS must articulate a clear vision for the future of value-based payment. In particular, the vision must align across all publicly financed health care, driving change beyond Medicare and Medicaid. Second, CMS must dramatically simplify the current value-based payment landscape and engage late-adopting providers. Third, for health systems already participating in value-based payment, CMS must accelerate the movement from upside-only shared savings to risk-bearing, population-based alternative payment models while curtailing the ability of providers to opt out of value-based payment altogether. Fourth, CMS must not only pull providers toward advanced alternative payment models, but also structure incentives to push providers away from fee-for-service payment. Finally, achieving health equity must be a central feature and goal of value- based payment. Taken together, these five recommendations provide a path toward widespread adoption and success of alternative payment models, producing better health outcomes for all Americans, reducing wasteful inefficiencies and health disparities, and more effectively stewarding taxpayer funds to support other national priorities.
Introduction: A Decade of Movement from Volume to Value
Since the passage of the Affordable Care Act (ACA) in 2010, the Centers for Medicare and Medicaid Services (CMS) has sought to transform U.S. health care from a system that incentivizes volume to one that rewards value. A key part of this strategy has been shifting from fee-for-service (FFS) payment to mechanisms that link provider reimbursement to improved quality and reduced costs. In 2015, Health and Human Services (HHS) Secretary Sylvia Burwell publicly committed CMS to tying at least 90% of traditional Medicare fee-for-service payments to quality by 2018.1
However, simply adding bonuses and penalties to fee-for-service payments is not enough to transform a system with historically high prices and inefficient care processes. Therefore, CMS has also developed advanced alternative payment models (APMs) that hold providers financially accountable for the quality and cost of care delivered to patients. These APMs include accountable care organizations (ACOs), episode- based payment models, Comprehensive Primary Care models, and other arrangements. Beyond committing to tying 90% of traditional Medicare fee-for-service payments to quality, CMS also sought to have at least half of payments flowing through APMs by 2018. According to the latest available data, while CMS has successfully tied 90% of payments to value, only about 40% flowed through APMs.2
However, the transition to a health care system that rewards value has slowed in recent years, and the promise of curtailing health care spending while also improving quality has remained elusive. Indeed, quality of care remains variable across health care settings with ongoing unnecessary utilization, low rates of compliance with recommended care, and inequities in health and health care. Meanwhile, though per-beneficiary spending growth in Medicare and Medicaid has slowed, aggregate spending continues to rise due to the aging population and expanded program eligibility. This will ultimately result in increasing per-enrollee costs3 and will contribute to the expected insolvency of the Medicare Trust Fund in 2024. In addition, without increased adoption of alternative payment models into the commercial market, where per-enrollee costs continue to outstrip inflation and wage growth, health care spending will continue to grow.4 The combination of quality and fiscal concerns require renewed focus on improving the value of health care for all Americans.
A Decade of Innovation
The 2010s produced many value-based programs, including Medicare’s flagship Shared Savings Program (MSSP) ACOs established under the ACA. Others were established through regulation, primarily by CMS’s Center for Medicare and Medicaid Innovation (CMMI), which has developed and tested dozens of alternative payment models. Commercial payers have followed Medicare’s lead, launching APMs with tailored episode and population-based models. After a decade of innovation, it is time to take stock of how successful these efforts have been in transforming health care payment and delivery.
Where We Are Now: Adoption of Value-Based Payment
The wide variety of current payment models may be categorized along a continuum, from legacy fee-for- service to global capitated payment. The Health Care Payment Learning & Action Network (HCP-LAN) defines four broad categories of payment (adapted in Table 1).2 Efforts to promote value-based payment focus on moving as many providers and as much revenue as possible to the third and fourth categories.
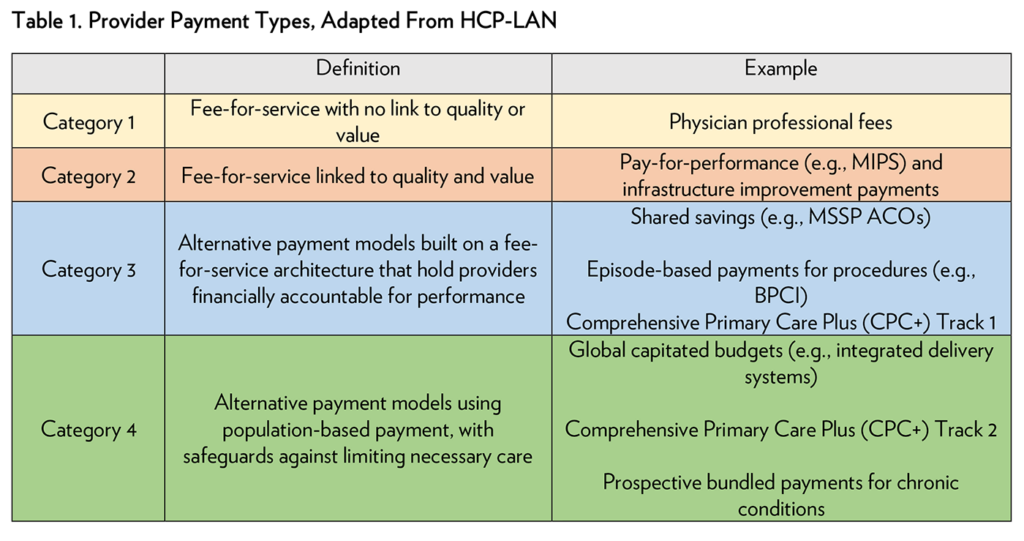
In 2018, fee-for-service with no link to quality or value still accounted for nearly 40% of all insurer payments, and the majority of payments in Medicaid and commercial insurance (Table 2). Medicare and Medicare Advantage have had more success in moving away from fee-for-service, although just a small fraction of these payments is in APMs with population-based payments.

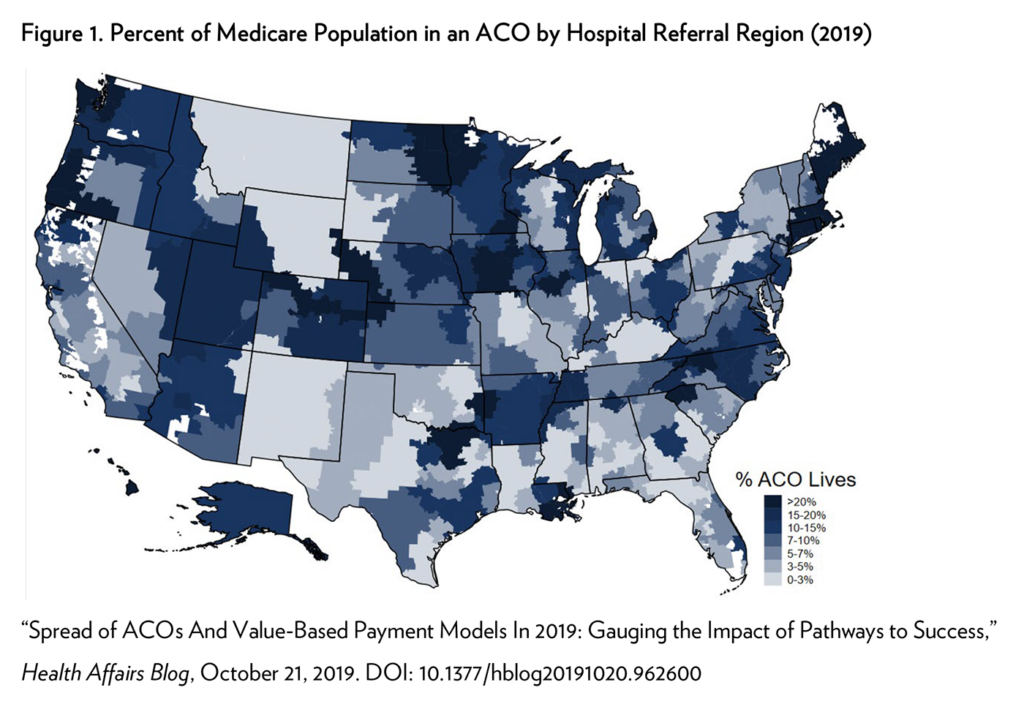
Furthermore, progress remains uneven across providers, geographic areas, and different APMs. In Medicare, most provider participation in population-based models is concentrated in the Medicare Shared Savings Program (MSSP). In 2020, roughly 500 MSSP ACOs served over 11 million Medicare beneficiaries (about 20% of all enrollees). MSSP participation is lower in many southern states and rural areas more broadly (Figure 1).
While patients in ACOs tend to have a higher clinical risk, providers in communities serving populations with social risk factors are less likely to participate in ACOs.5, 6 This may be, in part, because care for populations with high social risk is typically concentrated within a subset of providers, such as Federally Qualified Health Centers (FQHCs). More troublingly, some ACO models may emphasize reducing wasteful utilization, but for many populations the primary problem is under-utilization and underspending.
Similarly, most episode-based payment in Medicare is concentrated in the Bundled Payments for Care Improvement (BPCI) Advanced program. In the first performance year of BPCI Advanced (2018-2019), 22% of eligible hospitals and 23% of eligible clinicians participated in the program, which paid for 16% of potential episodes. While these adoption rates were higher than the previous iterations of BPCI, most hospitals that expressed interest did not ultimately enroll. BPCI Advanced hospitals were more likely to be urban, larger, and non-profit.7 Therefore, to the extent there are improvements in quality or efficiency, patients in rural areas with smaller health systems may be left behind.
While adoption of APMs has increased over time, many clinicians remain suspicious and hesitant to participate in any value-based payment.8 Most providers who do participate in value-based payment choose arrangements without downside financial risk, rather than making the jump to advanced APMs. In 2020, 37% of Medicare MSSP ACOs took on downside risk, up from less than 10% in 2017.9,10 In 2021, 41% of MSSP ACOs appear to be taking on downside risk, but the number of program participants and attributed beneficiaries has declined.9,11
Where We Are Now: Efficacy of Value-Based Payment and Health Disparities
The past decade of experimentation with APMs has had successes and failures. But it has provided proof-of- concept that if designed well, APMs are capable of driving cost savings and value improvements. There have been notable successes with the more advanced models that shift greater accountability onto providers, particularly those that do so over longer time horizons. Critics of value-based payment argue the movement is largely a disappointment, with only a small number reducing costs for Medicare, and many generating substantial losses.12 Observers are right to note that the current APM landscape includes many underperforming models, which have failed to produce the desired practice transformation. However, a decade of middling results does not imply that CMS should abandon value-based payment. The decade of experimentation has produced the necessary knowledge to design and implement APMs to transform health care delivery. We must build upon the most successful APMs and phase out those that have not delivered on their promise.
To date, the savings and quality gains from alternative payment models have been inconsistent and modest (Table 3).13-24 Bundled payment models have produced modest per-episode savings for surgical procedures, most notably lower extremity joint replacements. Bundled payments have produced smaller savings for select medical conditions, such as congestive heart failure, and no savings for other conditions, such as cancer and acute myocardial infarctions. There is no clear evidence of improvements to health equity.
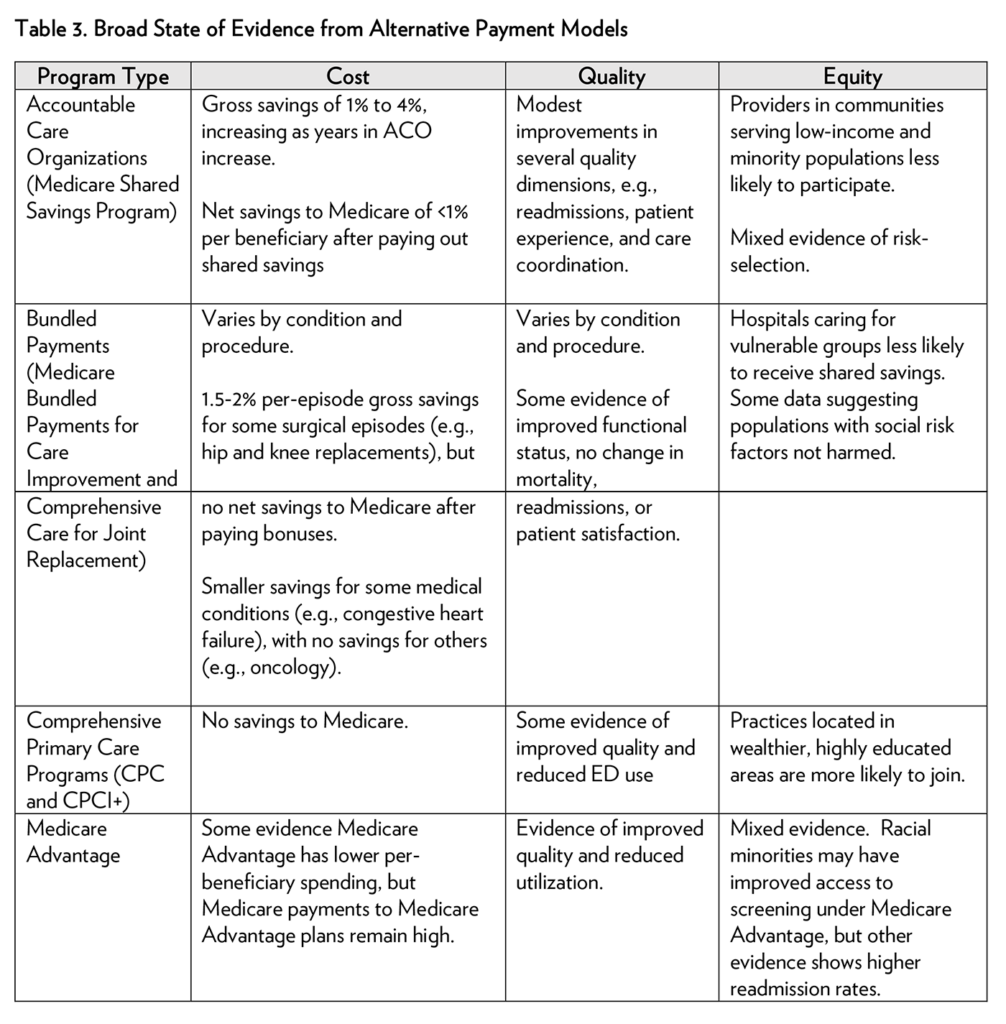
Population-based ACOs have generated modest per-beneficiary savings, with improvements along several quality dimensions. Evaluations suggest that physician-led ACOs have produced greater savings than hospital- led ACOs by reducing hospitalizations, and these savings increase the longer participants remain in the program. Hospital-led ACOs face conflicting incentives: lost admission revenues wipe out the shared savings earned through reducing hospitalizations. Therefore, hospital-led ACOs have focused on reducing post-acute care spending. While models targeting high-cost populations (e.g., those with end-stage renal disease) have generated the most savings, some evidence suggests that this is attributable to risk selection and regression to the mean. While evidence suggests some forms of commercial and Medicaid ACOs can reduce cost and improve quality, overall, there is much less evidence related to commercial and Medicaid ACOs.25, 26
With a small number of exceptions, value-based payment has yet to improve (or even explicitly address) access to care or health outcomes for populations with social risk factors, including racial and ethnic minorities, rural populations, and individuals with disabilities. Despite a growing recognition of these health care disparities, they persist across all payers. In most cases, CMS has focused on monitoring the unintended effects of value-based payment among populations with social risk factors. But the persistence of health inequities and disparities indicate systemic bias and underperformance in the health care system, and value-based payment must address those issues as key drivers of access and quality. To achieve health equity, value-based payment must directly address systemic racism. It must also increase its focus on measuring racial disparities and linking those data with financial outcomes. The COVID-19 pandemic’s disproportionate impact on low-income and minority communities underscores the need to make equity a core focus of value-based payment.
Challenges Remain for the Future of Value-Based Payment
What have we learned from this decade of innovation? While the last decade of APM experimentation includes both successes and failures, there are some lessons about what works. Some bundled-payment programs and ACOs have proven capable of reducing costs and improving the value of care delivered. Programs that use two-sided risk (i.e., shared savings and losses) appear to have the greatest impact.27 Successful value-based payment transitions take time; the savings and practice transformations from APMs take years of experience and investment to pay off.24 For independent physician groups and providers unwilling to take on value-based payment on their own, conveners with greater risk appetite and experience in value-based payment may be useful shepherds.
Underperforming models yield important insights. For example, alternative payment models must focus on optimizing shared decision-making tools and health IT infrastructure. Generous fee-for-service payment blunts the adoption of and effect of APMs, and federal efforts to reduce the draw of fee-for-service have so far been underpowered for the task. Therefore, the next decade of payment transformation must focus on expanding the most effective APMs that utilize two-sided risk, engaging more providers, and retaining current APM participants while graduating them to high-powered programs.
There are several challenges to these goals. The extensive administrative complexity of the value-based payment landscape remains a significant barrier to participating in APMs and to evaluating each model. Traditional fee-for-service remains alluringly profitable for providers, creating ambivalence for those weighing the tradeoffs of investing in traditional vs. risk-bearing business models and enabling late adopters to “wait out” payer interest in APMs. Many providers on the road to value-based payment seem unable or unwilling to make the transition from upside risk-only to fully accountable care. Advanced models have not been developed or implemented with a focus on health equity. Going forward, CMS must confront these challenges with a cohesive strategy to improve APM performance and accelerate the use of advanced APMs.
Goals for the 2020s: Articulate a Clear Vision for the Future of Value-Based Payment Across All Publicly Financed Health Care
Over the past decade, CMS and CMMI have focused on experimentation, generating dozens of alternative payment models with hundreds of tracks. It is time for CMS to lead with a strategic vision for the U.S. health care system and a publicly available path to executing that vision, as well as a carefully managed, straightforward, and sustainable APM portfolio.
The Case for an Overarching Framework
Excess experimentation has costs. Many APMs overlap both at the provider and beneficiary level, sometimes competing with each other. For providers not yet engaged in any value-based payment, the increasingly complex APM landscape dissuades adoption. Complexity encourages providers to chase small pools of shared savings, rather than systematically transform their practice. Overlapping models make it difficult to parse individual model effects on cost and quality, frustrating efforts to identify and expand the highest-performing models. With little guidance on the types of value-based models CMS will sustain over the long term, health systems are unsure of how to invest for optimal transformation and return on investment. Over the next decade, providers need guidance and assistance, not experiments. Instead of a narrow focus on individual models, CMS must begin to evaluate regularly the effect of the whole APM portfolio against expectations, within a guiding framework.
A Proposed Path Forward
CMS must articulate a vision for health care delivery and payment for 2030 that includes a long-term plan for the evolution of APMs, the coordination of models’ financial designs, and mandatory participation that moves to eliminate risk-free fee-for-service arrangements. A clear strategy and set of goals would allow CMS to slow the introduction of new models, evaluate the projected and observed performance of existing models, and phase out underperforming initiatives. The framework should map different models to provider types (e.g., health systems, specialists, and primary care groups, as shown in Figure 2).
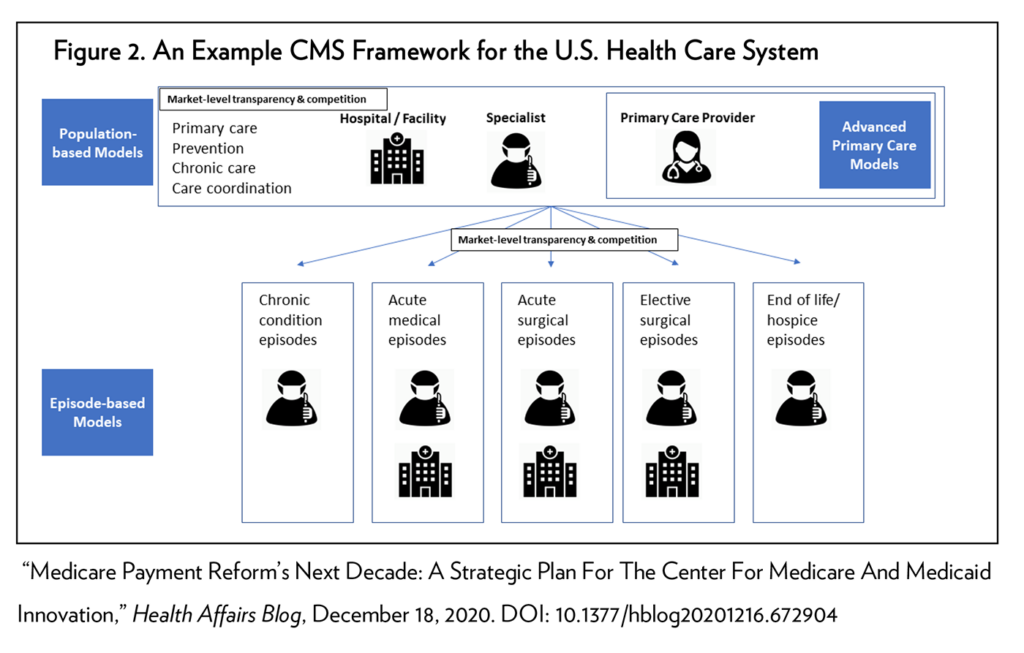
As illustrated above, for prospectively attributed beneficiaries, groups of providers could be accountable for total cost of care (through population-based payment via a health system, an ACO, or another convener), with procedure-based specialists paid through bundled payments. Primary care providers could be paid under advanced primary care models that include capitated fees for care management activities. Benchmarks for episode and populated-based payment could be based on average costs in a market, rather than on each provider’s past performance. Mandatory population-based payments would be the linchpin of this strategy, because they can mitigate risk selection and promote care coordination.
Improving model performance will likely require provider competition at the market level, which in turn demands substantial reforms to performance benchmarking. The current approach to generating cost and quality baselines uses historical provider performance, with regular re-balancing. This mechanism generates a “race to the bottom” and penalizes providers that were already efficient. In contrast, setting performance baselines based on regional trends generates stronger incentives for practice transformation with transparent goals. However, regional benchmarking is only possible if CMS puts a greater emphasis on mandatory programs to generate an even playing field.
CMS Needs to Manage Its Portfolio Strategically
To support its strategic vision, CMS should bring a portfolio-based approach to its value-based payment initiatives. The portfolio approach treats new payment models as a series of investments across APM programs, with specific allotments based on desired high-level goals, such as reducing per-beneficiary costs, improving value, and addressing health equity. Such a division of investments would guide how CMS allocates resources and measures success. The benefits to a long-term portfolio approach are manifold. First, a long-term commitment to a specific set of investments helps guard against shifting political goals. Second, it provides clarity to providers about the types of value-based program initiatives that are most suitable for investment. Finally, it allows for a clear accounting of success and failures in value-based payment, separating wheat from chaff.
As an illustration, CMS could allot 40% of its APM portfolio (measured either in investment dollars or number of participating providers or beneficiaries) to a selection of models that are most likely to produce significant value improvements and 30% to programs aimed at improving outcomes for populations with social risk factors. A fifth of the portfolio could focus on novel experiments that are not payment models, but can still yield savings (e.g., addressing prescription drug costs). A tenth of the portfolio could aim to reduce out-of-pocket costs. Furthermore, health equity should be considered across all portfolio areas. Such a pre-determined allocation would work in parallel with the larger strategic vision for national practice transformation, and it could be adapted based on the evolution of evidence for APMs.
Goals for the 2020s: Simplify the Value-Based Payment Landscape, Reduce Administrative Barriers for Late-Adopters, and Graduate Providers to Advanced Risk-Bearing Arrangements
Accelerating the transition to value-based payment requires both drawing in late adopters and moving current program participants to higher-risk APM contracts. To expand and entrench APMs, CMS must focus on aligning APMs across payers, simplifying the administration of APMs, reforming the way performance benchmarks are set, requiring participation in APMs when possible, and reducing the appeal of traditional fee- for-service when it is not.
Pulling Providers in Through Alignment of APM Goals Across Payers
Adoption and coordination of APMs across payers would have significant benefits by increasing providers’ total share of revenue flowing through APMs, thus creating a stronger business case for accelerating practice transformation. However, HHS has not adequately promoted APM adoption beyond Medicare. Over the next decade, policymakers should promote national transformation and alignment by leveraging the full range of federally funded health care programs.
The private sector accounts for the largest share of national health care spending due to its high reimbursement rates. However, as shown in Table 2, commercial insurers have been slow to shift to value-based payment. For APMs to be successful, they must be aligned and harmonized across payers, service lines, and health plans. The federal government and CMS can lead this movement by aligning value-based payment in public programs with those in private programs that receive federal subsidies. This includes Medicare, TRICARE, the Veterans Health Administration, the Federal Employee Health Benefits Program, commercial plans sold on ACA exchanges, Medicaid, and managed care in both Medicare and Medicaid. For example, HHS should require that insurance plans sold on the ACA exchanges commit to similar APM adoption and structure as Medicare in order to draw premium subsidies. Similarly, Medicaid managed care organizations must use APMs in order to draw federal funds, and Medicare Advantage bids should be contingent on a meaningful percentage of the plan’s provider network participating in APMs.
While the government may move many payers in similar directions, it must balance harmonization with being overly prescriptive. Medicaid, Medicare, and commercial insurance markets serve different populations, which may require different spending priorities and quality metrics. Aligning goals across programs should be flexible enough to allow these differences to emerge within a specified payment structure. However, aligning goals for APMs should not further entrench inequities by taking as a given that quality outcomes should be worse for populations with high social risks. Therefore, CMS should spearhead the development of multi-stakeholder standards, with template models (e.g., surgical bundles and capitated primary care programs) and adaptations for different populations, setting realistic goals without entrenching current inequities. Where appropriate, it should promote state or regional multi-payer models that can push providers in a coordinated direction. The overall goal is to increase the share of revenue tied to quality past the point of no return, which requires commercial buy-in.
Pulling Providers in Through Administrative Simplification
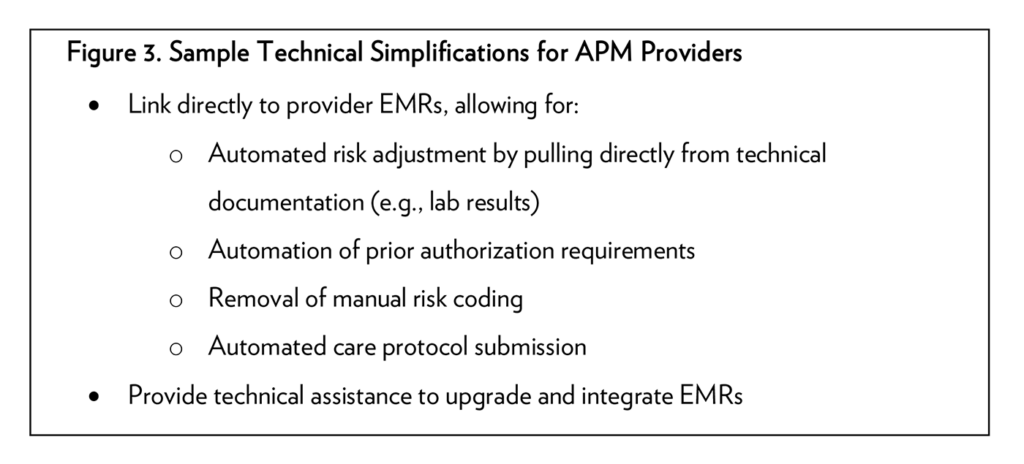
CMS must also simplify the administrative burden of alternative payment models. As noted, regional benchmarking can achieve substantial simplification for providers. Additionally, APMs must lock in providers with more attractive multi-year commitments. Annual recommitments to APMs can result in substantial churn of providers participating in APMs and beneficiaries attributed to APMs, creating few incentives for providers to make long-term investments in efficiency. In contrast, long-term contracts—such as five-year agreements— signal a commitment to program success from CMS, and encourage providers to make greater technical and programmatic investments in early years, with expected savings accruing in later years. Long-term contracts should include multi-year beneficiary attribution—unless beneficiaries opt out or move—which allows providers to cement care relationships and truly reap the returns on care management investments. Along with long-term contracts and mandatory participation, CMS should prioritize identifying and implementing technical changes to the structure of APMs to facilitate model adoption (Figure 3).
Pulling Providers in Through Mandatory Participation in APMs
CMS must move away from voluntary provider participation in APMs, and work with providers and conveners to implement mandatory participation whenever feasible. The last decade has demonstrated bipartisan support for many mandatory programs, which have at least four advantages. First, mandatory participation simplifies the adoption of new payment models for providers and produces fair competition when benchmarks are set at the regional level. Second, mandatory programs mitigate undesirable dynamics that occur when markets segment into value-based and fee-for-service providers, such as risk selection of patients by providers participating in APMs. Third, they are the most efficient way to bring in late adopters. Finally, they allow for better control over evaluation, which in turn produces robust results, allowing the best versions of models to emerge and diffuse more rapidly.
Pulling Providers in by Reducing the Draw of Fee-for-Service
In some cases, requiring participation in APMs is not possible. In those cases, increasing the voluntary adoption of risk-bearing APMs requires reducing the attractiveness of fee-for-service arrangements. First, CMS must re- evaluate the current physician fee schedule, which is biased towards procedures, overvalues several specialty procedure codes, and undervalues primary care. CMS must reprice the most used billing codes based on value, adjusting payments based on actual work time as documented in established research. CMS must also rebalance fees paid for inpatient hospital diagnosis-related groups (DRGs) and medical supplies (e.g., oxygen and blood).
The impact of these reforms would reverberate throughout the private market.
Negotiations between commercial payers and providers use CMS fees as a reference point, often reflecting Medicare fees with relative multipliers. Therefore, rebalancing the CMS fee schedule will not only pull providers to APMs within Medicare, but it will also improve the capacity of private payers to engage in APMs with health systems and physicians.
CMS can also leverage consumer demand to reduce the attractiveness of fee-for-service, driving beneficiaries to providers participating in APMs, and, more importantly, to high-performing providers. For example, CMS could offer greater flexibility for telehealth waivers for providers in APMs and reduce patient cost-sharing for specialists who utilized bundled payments. These mechanisms would discourage continued reliance on traditional fee-for-service by making voluntary participation in APMs more economically attractive, which will encourage broad practice transformation.
Goals for the 2020s: Value-Based Payment Focused on Equity and Populations with Social Risk Factors
Far too often, the design of value-based contracts fails to account for health inequities or the possible effects of value-based payment on health disparities. With a few exceptions, such as the ACO Investment Model, most alternative payment models do not have an explicit goal of reducing health disparities. As a result, APMs may penalize practices if they care for patients with high social risk. Rather than targeting health equity, health disparities are considered as an afterthought in the evaluation, with monitoring to make sure spending reductions and quality improvement do not inadvertently worsen access and care of populations with social risk factors. Going forward, APMs should proactively promote equity with design decisions that treat reducing disparities as a priority.
Improving Health Equity is a Goal of Value-Based Payment
Several mechanisms can tie alternative payment models to health equity. In most cases, APMs can include explicit, direct funding that targets the care of populations with social risk factors, including funding for community health workers, community-based services, and teams that integrate health and social services. APMs can require participants to screen for social risk factors, track those data in electronic health records, and address those risk factors. Stratifying outcomes by race or other sources of social risk would allow CMS to tie shared savings bonuses to reducing disparities, publicly reporting those data and rewarding providers that close gaps. Consistently implementing these types of reforms across APMs in Medicare, Medicaid, and ACA exchange plans would offer providers a meaningful business case for addressing disparities.
In addition to specific financial incentives, there are also several non-financial policies CMS can put in place to address health equity. For example, Medicare and other federal payers can require that ACOs produce equity impact statements that outline the current state of health equity in the beneficiary population, and how the ACO plans to reduce disparities in outcomes for populations with social risk factors. Impact statements should include measurable goals, clear metrics for success, and a commitment to making this information publicly available. CMS should also improve its approach to measuring social risk, which may require intra-agency coordination to develop new standards for data collection and measure definitions. Furthermore, CMS must lead the development of validated measures of health equity, which are scarce. Finally, all publicly reported patient outcomes, such as readmission rates, should be stratified by social risk factors. These reforms would also reduce the likelihood that providers in APMs might avoid caring for populations with social risk factors.
Integrating Social Services into Health Care Delivery, With a Focus on Medicaid
Ultimately, patients’ outcomes are influenced by more factors beyond health care services. Unstable housing, food insecurity, limited educational attainment, and poverty drive poor health outcomes. Policymakers can use APMs and the full suite of federally financed health care to encourage providers to integrate health care delivery with social services that address needed housing, food, and transportation, whether delivered by states, the federal government, or independent non-profits.
Thus far, CMS has taken a limited approach to addressing social determinants of health, such as allowing Medicare Advantage plans to pay for food and transportation services. Over the next decade, across all APMs, CMS must explicitly require providers to connect beneficiaries to other social support programs for which they are eligible and provide guidance and funding for APMs to close gaps related to social determinants of health.
The largest opportunity to do so lies in Medicaid, but these efforts should not be limited to Medicaid. CMS should provide clear guidance that allows Medicare, Medicaid (beyond the use of waivers), and Medicaid managed care organizations to spend federal funding on social supports—either directly or through contracted agreements with social service providers—and to include capitated payment to providers for care management activities.
Allowing for greater spending on social supports through federal insurance will also require greater accountability. Specifically, Medicaid must become a one-stop shop for all means-tested social welfare programs. Federal funding for state Medicaid programs and Medicaid managed care organizations should be contingent on actively enrolling beneficiaries and their dependents in other programs for which they qualify, such as housing vouchers, supplemental nutrition assistance (SNAP), or Head Start. CMS should provide technical assistance to states to implement and support these efforts.
Conclusion
In the decade since the passage of the Affordable Care Act, the health care system has reached a series of important milestones in its shift to paying for value. Led by CMS, a growing share of payers have moved away from outmoded fee-for-service payment. More providers than ever before are engaged in some form of quality-linked payment, and a smaller cadre have begun experimenting with advanced forms of population- based payment and large-scale practice transformation.
We now need a more focused, whole-of-government push toward a high-quality, efficient system. The persistence of health disparities, uneven quality, and continued rise of health care costs, and the concomitant threat to federal and state budgets, requires renewed focus on spreading the adoption of advanced forms of alternative payment models. These models must move from experimentation to an entrenched, nationwide standard.
The past decade of experimentation shows that alternative payment models as currently implemented are not driving large-scale, systemic change. But a careful study of the lessons from both successful and underperforming models suggests that properly designed APMs can yield improvements in value through cost reductions and quality improvements. The next decade must put those lessons into practice by engaging late adopters, ramping up already adopted and successful APMs, driving payment and practice transformation in commercial insurance, and integrating equity front and center in value-based payment. The goal of a sustainable health care system that pays for better quality, equity, and efficiency is both audacious and fully achievable.
References
- Burwell, S. M. (2015). Setting value-based payment goals–HHS efforts to improve U.S. health care. N Engl J Med, 372(10), 897-899. doi:10.1056/NEJMp1500445
- Measuring Progress: Adoption of Alternative Payment Models in Commercial, Medicaid, Medicare Advantage, and Traditional Medicare Programs. Health Care Payment Learning & Action Network. Retrieved from http://hcp-lan.org/workproducts/apm-methodology-2019.pdf
- Martin, A. B., Hartman, M., Lassman, D., Catlin, A., & National Health Expenditure Accounts, T. (2021). National Health Care Spending In 2019: Steady Growth For The Fourth Consecutive Year. Health Aff (Millwood), 40(1), 14-24. doi:10.1377/hlthaff.2020.02022
- Claxton, G., Damico, A., Rae, M., Young, G., McDermott, D., & Whitmore, H. (2020). Health Benefits In 2020: Premiums In Employer-Sponsored Plans Grow 4 Percent; Employers Consider Responses To Pandemic. Health Aff (Millwood), 39(11), 2018-2028. doi:10.1377/hlthaff.2020.01569
- Werner, R. M., Kanter, G. P., & Polsky, D. (2019). Association of Physician Group Participation in Accountable Care Organizations With Patient Social and Clinical Characteristics. JAMA Netw Open, 2(1), e187220. doi:10.1001/jamanetworkopen.2018.7220
- Yasaitis, L. C., Pajerowski, W., Polsky, D., & Werner, R. M. (2016). Physicians’ Participation In ACOs Is Lower In Places With Vulnerable Populations Than In More Affluent Communities. Health Aff (Millwood), 35(8), 1382-1390. doi:10.1377/hlthaff.2015.1635
- Dummit, L. A., Marshall, J., Bergman, S., Cammarota, R., Chander, R., Collins, T., . . . Josepth-King, M. The Lewin Group. CMS Bundled Payments for Care Improvement Advanced Model: Year 1 Evaluation Annual Report. Retrieved from https://innovation.cms.gov/data-and-reports/2020/bpciadvanced- firstannevalrpt
- Bethke, M., Gordon, R., Elsner, N., & Varia, H. (2020). Equipping physicians for value-based care: What needs to change in care models, compensation, and decision-making tools? Retrieved from https://www2.deloitte.com/us/en/insights/industry/health-care/physicians-guide-value-based-care- trends.html
- Shared Savings Program Fast Facts — As of January 1, 2021. U.S. Centers for Medicare & Medicaid Services. Retrieved from https://www.cms.gov/files/document/2021-shared-savings-program-fast-facts.pdf
- Sullivan, G., Feore, J., & Seidman, J. (2020). Avalere. MSSP Sees Continued Growth in Downside Risk ACOs. Retrieved from https://avalere.com/insights/mssp-sees-continued-growth-in-downside-risk- acos
- Verma, S. (2020). Number Of ACOs Taking Downside Risk Doubles Under ‘Pathways To Success’. Health Affairs Blog. doi:10.1377/hblog20200110.9101
- Smith, B. (2021). CMS Innovation Center at 10 Years – Progress and Lessons Learned. N Engl J Med. doi:10.1056/NEJMsb2031138
- Liao, J. M., Navathe, A. S., & Werner, R. M. (2020). The Impact of Medicare’s Alternative Payment Models on the Value of Care. Annual Review of Public Health, 41(1), 551-565. doi:10.1146/annurev-publhealth- 040119-094327
- Agarwal, R., Liao, J. M., Gupta, A., & Navathe, A. S. (2020). The Impact Of Bundled Payment On Health Care Spending, Utilization, And Quality: A Systematic Review. Health Aff (Millwood), 39(1), 50-57. doi:10.1377/hlthaff.2019.00784
- Navathe, A. S., Emanuel, E. J., Venkataramani, A. S., Huang, Q., Gupta, A., Dinh, C. T., . . . Liao, J. M. (2020). Spending And Quality After Three Years Of Medicare’s Voluntary Bundled Payment For Joint Replacement Surgery. Health Aff (Millwood), 39(1), 58-66. doi:10.1377/hlthaff.2019.00466
- Rolnick, J. A., Liao, J. M., Emanuel, E. J., Huang, Q., Ma, X., Shan, E. Z., . . . Navathe, A. S. (2020). Spending and quality after three years of Medicare’s bundled payments for medical conditions: quasi- experimental difference-in-differences study. BMJ, 369, m1780. doi:10.1136/bmj.m1780
- Kim, H., Meath, T. H. A., Dobbertin, K., Quinones, A. R., Ibrahim, S. A., & McConnell, K. J. (2019). Association of the Mandatory Medicare Bundled Payment With Joint Replacement Outcomes in Hospitals With Disadvantaged Patients. JAMA Netw Open, 2(11), e1914696. doi:10.1001/jamanetworkopen.2019.14696
- Fraze, T. K., Fisher, E. S., Tomaino, M. R., Peck, K. A., & Meara, E. (2018). Comparison of Populations Served in Hospital Service Areas With and Without Comprehensive Primary Care Plus Medical Homes. JAMA Netw Open, 1(5), e182169. doi:10.1001/jamanetworkopen.2018.2169
- Winblad, U., Mor, V., McHugh, J. P., & Rahman, M. (2017). ACO-Affiliated Hospitals Reduced Rehospitalizations From Skilled Nursing Facilities Faster Than Other Hospitals. Health Aff (Millwood), 36(1), 67-73. doi:10.1377/hlthaff.2016.0759
- Newhouse, J. P., & McGuire, T. G. (2014). How successful is Medicare Advantage? Milbank Q, 92(2), 351- 394. doi:10.1111/1468-0009.12061
- McWilliams, J. M., Landon, B. E., Chernew, M. E., & Zaslavsky, A. M. (2014). Changes in patients’ experiences in Medicare Accountable Care Organizations. N Engl J Med, 371(18), 1715-1724. doi:10.1056/NEJMsa1406552
- Li, Y., Cen, X., Cai, X., Thirukumaran, C. P., Zhou, J., & Glance, L. G. (2017). Medicare Advantage Associated With More Racial Disparity Than Traditional Medicare For Hospital Readmissions. Health Aff (Millwood), 36(7), 1328-1335. doi:10.1377/hlthaff.2016.1344
- Racial, Ethnic, and Gender Disparities in Health Care in Medicare Advantage. CMS Office of Minority Health and RAND Corporation. Retrieved from https://www.cms.gov/About-CMS/Agency- Information/OMH/Downloads/2018-National-Level-Results-by-Race-Ethnicity-and-Gender.pdf
- McWilliams, J. M., Hatfield, L. A., Landon, B. E., Hamed, P., & Chernew, M. E. (2018). Medicare Spending after 3 Years of the Medicare Shared Savings Program. N Engl J Med, 379(12), 1139-1149. doi:10.1056/NEJMsa1803388
- Song, Z., Ji, Y., Safran, D. G., & Chernew, M. E. (2019). Health Care Spending, Utilization, and Quality 8 Years into Global Payment. N Engl J Med, 381(3), 252-263. doi:10.1056/NEJMsa1813621
- McConnell, K. J., Renfro, S., Chan, B. K. S., Meath, T. H. A., Mendelson, A., Cohen, D., . . . Lindrooth, R. C. (2017). Early Performance in Medicaid Accountable Care Organizations: A Comparison of Oregon and Colorado. JAMA Internal Medicine, 177(4), 538-545. doi:10.1001/jamainternmed.2016.9098
- Final Rule Creates Pathways to Success for the Medicare Shared Savings Program. [Press release]. U.S. Centers for Medicare & Medicaid Services. Retrieved from https://www.cms.gov/newsroom/fact- sheets/final-rule-creates-pathways-success-medicare-shared-savings-program
Disclosure Statement
Dr. Werner reports receiving personal fees from Health Research & Educational Trust, FAIR Health, John Wiley & Sons, and University of Massachusetts Medical School-Baystate.
Dr. Emanuel reports receiving speaker’s fees from Kaiser Permanente Virtual Medicine, Wallace H. Coulter Foundation, Lake Nona Institute, Partners Chicago, Pepperdine University, Huron, American Case Management Association, Philadelphia Chamber of Commerce, Blue Cross Blue Shield Minnesota, UnitedHealth Group, Futures Without Violence, CHOP, Washington State Hospital Association, Association of Academic Health Centers, Blue Cross Blue Shield of Massachusetts, Lumeris, Roivant Sciences Inc, Medical Specialties Distributors LLC, Vizient University Healthcare System, Center for Neuro-Degenerative Research, Colorado State University, Genentech Oncology Inc, Council of Insurance Agents and Brokers, Grifols Foundation, America’s Health Insurance Plans, Montefiore Physician Leadership Academy, Greenwall Foundation, Medical Home Network, HFMA, Ecumenical Center–UT Health, American Academy of Optometry, Associação Nacional de Hospitais Privados, National Alliance of Healthcare Purchaser Coalitions, Optum Labs, Massachusetts Association of Health Plans, District of Columbia Hospital Association, Washington University, Optum, Brown University, America’s Essential Hospitals, National Resident Matching Program, Shore Memorial Health System, Tulane University, Oregon Health & Science University, McKay Lab, CBI, American Society for Surgery of the Hand, Association of American Medical Colleges, Johns Hopkins University, and BCBS. He also reports being a venture partner with Oak HC/FT; being on the board of Village MD and Oncology Analytics; and being a partner at Embedded Healthcare LLC and COVID-19 Recovery Consulting.
Dr. Pham reports receiving consulting fees from CityBlock, Coeur Value, and NAACOS.
Dr. Navathe reports receiving personal fees from Navvis Healthcare, Agathos, Inc., YNHHSC/CORE, Maine Health Accountable Care Organization, Maine Department of Health and Human Services, National University Health System -Singapore, Ministry of Health -Singapore, from Elsevier Press, Medicare Payment Advisory Commission, Cleveland Clinic, Analysis Group, VBID Health, personal fees and equity from Navahealth, and equity from Embedded Healthcare, and other from Integrated Services, Inc.