Health Equity | Improving Care for Older Adults
Blog Post
What’s Happening at Skilled Nursing Facilities on Day 20?
Medicare payment linked to high discharge rates of vulnerable patients
There’s something unusual happening on patients’ 20th day in skilled nursing facilities (SNFs). In a JAMA Internal Medicine study, Paula Chatterjee, Norma Coe, Rachel Werner, and colleagues found that more people were discharged on day 20 of their SNF benefit period than days 19 or 21. This pattern reflects how Medicare pays for postacute care at a SNF: for the first 20 days of care, Medicare covers 100% of a patient’s costs. On the 21st day, most patients must begin paying a daily copayment of over $150.
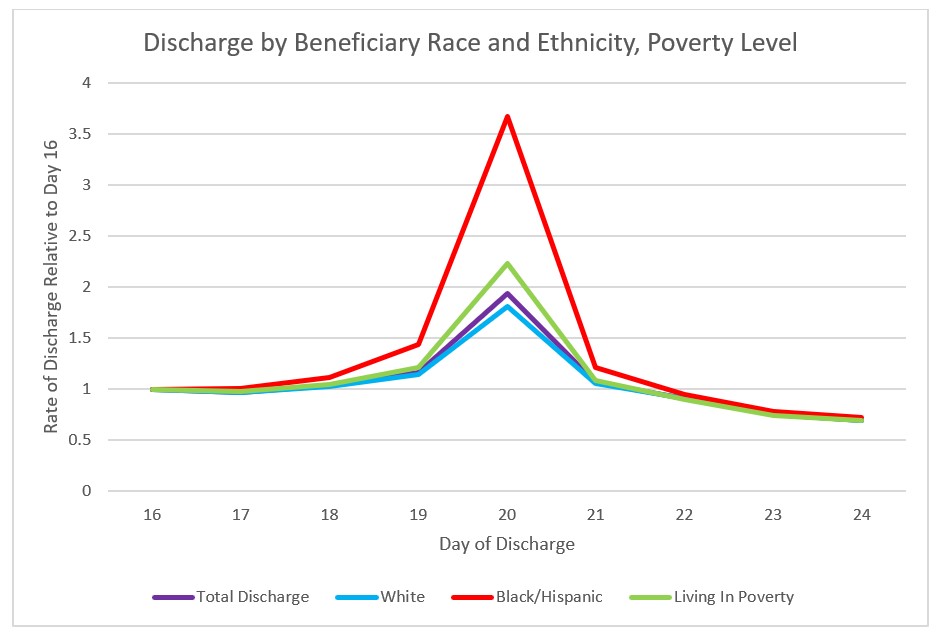
While there was a spike in discharges among all patient subgroups on day 20, the chart below demonstrates that discharged patients were more likely to be racial and ethnic minorities and live in high-poverty areas with higher unemployment rates. Discharge among black and Hispanic beneficiaries on day 20 compared to day 16 happened at a rate double that of white beneficiaries.
The results of this study raise more questions than they answer. Is the push to discharge patients on day 20 coming from the patient or the nursing facility? There are a few likely scenarios:
- Patients may be aware of the upcoming charge and choose to be discharged, rather than be burdened with the steep out-of-pocket cost of staying a few extra days.
- SNFs may be discharging these vulnerable patients early out of fear that they may not be able to pay, or that uncompensated care will lead to “bad debt.”
- SNFs may be keeping patients up to day 20 past the point of medical necessity to capitalize on guaranteed Medicare reimbursement.
While these findings do not entirely explain the racial/ethnic and socioeconomic divide among SNF discharges, they do demonstrate a higher discharge rate among vulnerable patients when Medicare stops paying. Current Medicare payment structures for SNF stays must be examined to ensure that they are not exacerbating existing inequalities and disadvantaging the patients most at risk. Researchers should continue to explore the relationship among Medicare payment, postacute care, and social determinants of health. You can read the full study here.