Blog Post
Penn LDI’s Top 10 Reads of 2018
What caught our readers’ attention
2018 was a year that defies easy categorization. In health policy, deep cynicism and hyperpartisanship often made evidence seem almost passé, a quaint paean to a time when research and data might contribute to a thoughtful national debate. But if you listened closely, you also heard not-so-faint rumblings of a desire to get past slogans and bitter divides, to find areas of common ground, and to use evidence to improve health and health care, even if only incrementally. In 2018, people flocked to LDI in record numbers, with more than 550,000 page views on our website. Our most popular content reflects this yin and yang of cynicism and hopefulness. If eyes (clicks) on the page are any indication, readers looked to LDI for straight talk about what is possible and likely in our present policy environment. Here we present our Top 10 reads of 2018.
By far, the most read (and downloaded) was this illustrated “special report” by Wharton professors Rob Burns and Mark Pauly that identified the top 10 candidates for BS in the health care industry. In their inimitable tongue-in-cheek way, Burns and Pauly lay waste to some trendy management concepts that have little to no evidence behind them. Rumor has it that BS 2.0 is in the works!
2. State Efforts to Close the Health Coverage Gap

We launched our partnership with United States of Care with this joint Issue Brief on prominent state efforts in Massachusetts, Vermont, Colorado, California, and Nevada to expand health coverage to the remaining uninsured. LDI Executive Director Dan Polsky and United States of Care Board Chair Andy Slavitt co-authored a Health Affairs blog post on the key insights and themes from the analysis. At the heart of this partnership is a deep commitment to finding common ground on expanding coverage, and a practical acknowledgement that states are more likely than the federal government to tackle coverage and access issues, at least in the next few years. Since our launch, the partnership produced another Issue Brief on how to define “affordability” in health care. Never let it be said that the partnership takes on the easy issues…
3. Penn Postdoctoral Researchers’ Study of Australian Gun Control Laws
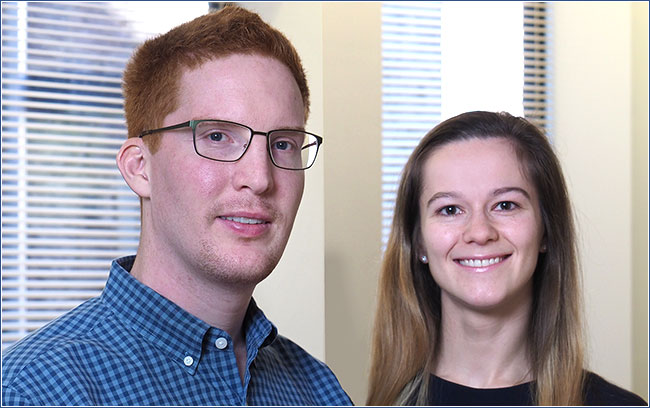
In the aftermath of the February 2018 school shooting in Parkland, Florida, we highlighted new research by Benjamin Ukert and Elena Andreyeva on the effects of strict gun control laws that Australia implemented after a mass shooting 22 years ago. Two papers point out the methodological challenges in evaluating the laws, and their conclusions that firearm-related deaths declined significantly after enactment (and no other mass shootings occurred). Although they were careful not to suggest that the findings were translatable to the United States, the attention these papers drew reflected a broader willingness to consider policies to reduce the level of firearm deaths and injury, a movement led by the Parkland survivors themselves.
4. Public Opinion and Health Reform
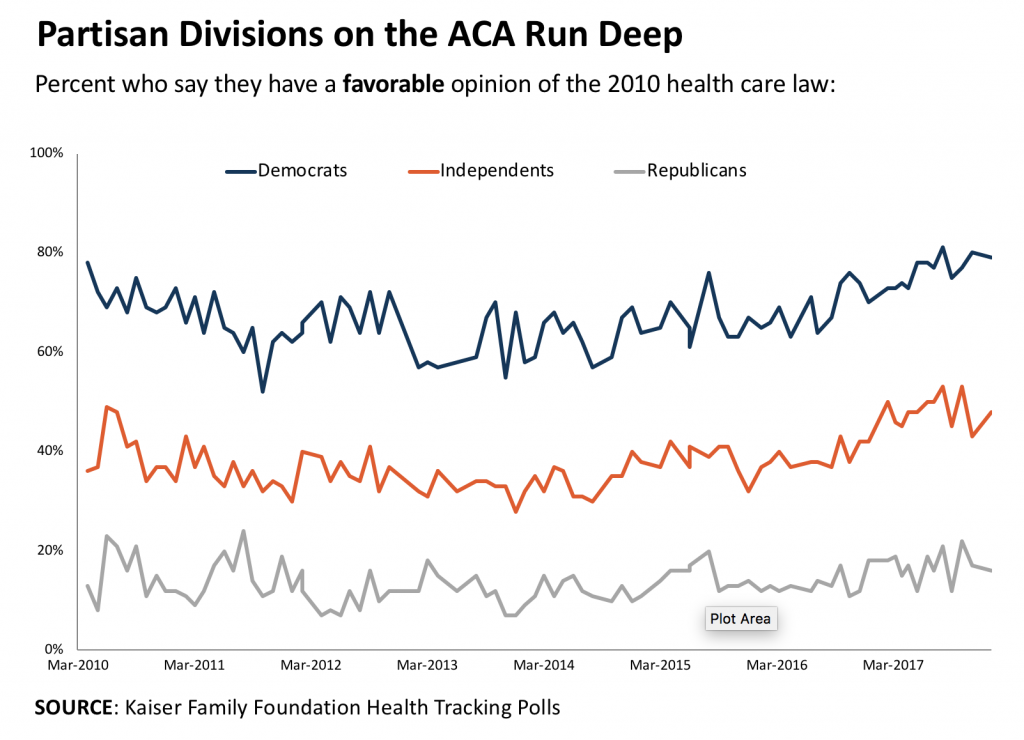
In a year characterized by continuing attempts to roll back or repeal the Affordable Care Act, our readers wanted to understand what the public thought about health care reform, and whether it had changed over time.In this blog post, we summarize the evidence from a talk by Mollyann Brodie of the Kaiser Family Foundation, who has been tracking public opinion on the ACA since its implementation. Her conclusion? “Democrats favored the ACA from day one (they still do); Republicans hated the ACA from day one (they still do); and independents seem to be in the middle.”
5. Report from the First National ‘Nudge Units in Health Care’ Symposium

“Think small,” attendees heard from leaders of Penn Medicine’s Nudge Unit, on how to apply behavioral economics insights within a health system. The two-day symposium drew executives and researchers from 22 health systems in the US and Canada, and featured a keynote by Cass Sunstein, author of the book, “Nudge.” This report captures the excitement and promise of small-scale efforts of the Nudge Unit, the Center for Health Incentives and Behavioral Economics, and Penn Medicine’s Center for Health Care Innovation that are having big results in terms of improving patient outcomes.
6. Medicaid Expansion and the Opioid Epidemic
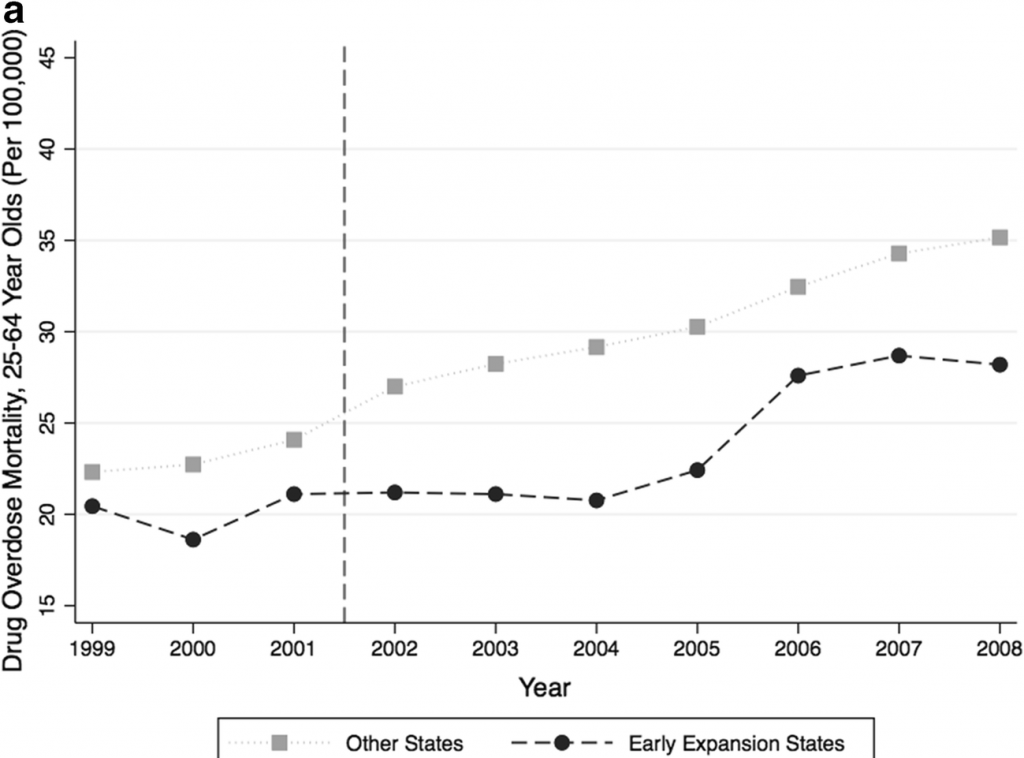
Cynicism and partisanship were on full display as a Senate report claimed that Medicaid expansion had fueled the opioid epidemic by increasing access to prescription opioids. This blog post pointed to the growing number of studies debunking this claim, including one by Paula Chatterjee and Atheendar Venkataramani. Instead, mounting evidence suggests that Medicaid expansion reduces mortality from drug overdoses and increases access to drug treatment.
7. The Future of Medicaid: State Legislator Views on Policy Waivers
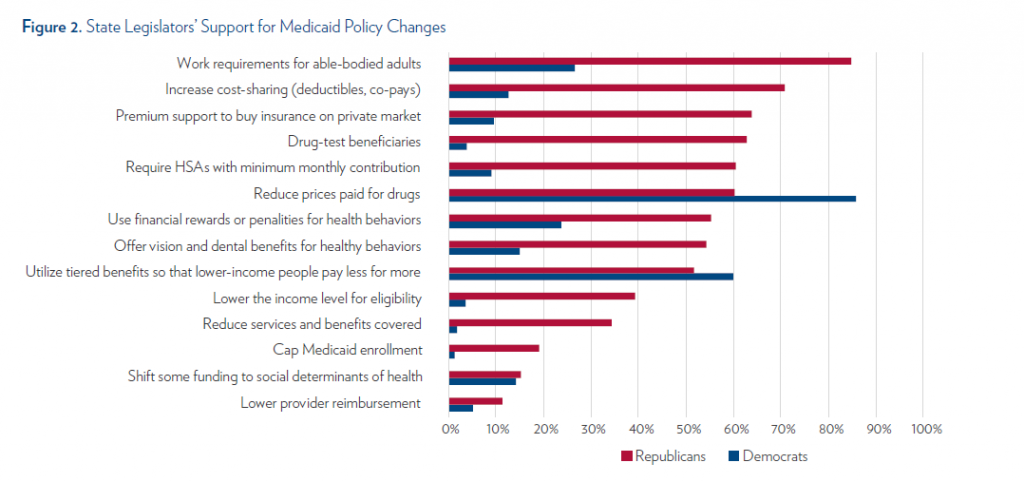
As the administration signaled increasing willingness to approve state-level waivers to the Medicaid program, it appeared that state legislators would have unprecedented leeway to experiment with new reforms. In research funded by LDI’s Policy Accelerator Program, Jane Zhu, Manik Chhabra, and Dave Grande surveyed state legislators to understand support for Medicaid policy changes and identified significant policy divides by party. However, they also identified areas of common ground, including support for reducing drug prices. The research was published in the Journal of General Internal Medicine and this Research Brief highlights its findings.
8. Community Health Care Worker Program Expands Beyond Penn

Seven years of careful research and structured implementation of a community health workers program has yielded impressive results in addressing the social determinants of health among low-income populations. Shreya Kangovi, director of Penn’s Center for Community Health Workers, briefly described these findings in a video and a blog post summarized the evidence to date. This article captures the history and current status of the program, which has spread to more than 20 institutions across the country. Kangovi lays out an important policy and business case. At a time when health spending for low-income Americans is increasingly on the chopping block, she says, “we can actually reduce spending for Medicaid while improving health rather than locking them out of coverage.”
9. Value Based Payment: Is This Time Actually Different?

Here they go again. In a Milbank Quarterly article, Rob Burns and Mark Pauly challenge the prevailing wisdom that payment and practice transitions are happening quickly, shifting financial risk to providers, and leading to higher quality, lower cost care. They provide historical context and a sweeping overview of studies to date to conclude that “the transformation from ‘volume to value’ appears to be driven more by ideology and aspiration than by evidence.” This blog post drew lots of attention to their suggestion to “curb your enthusiasm” about value-based payment.
10. Where Patients Go After Hospital Discharge: Trends in Post-Acute Care
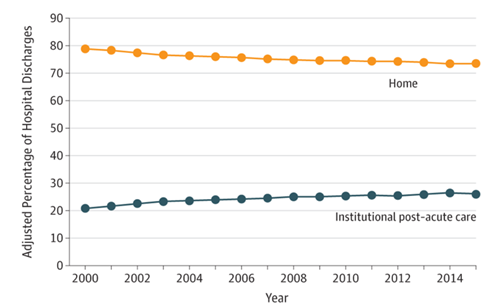
Medicare payment reforms such as readmissions penalties and bundled payments have made hospitals accountable for care beyond their walls. Surprisingly little attention has been paid to where patients go immediately after discharge. In a Research Letter in JAMA, Rachel Werner and R. Tamara Konetzka fill the gap by analyzing how post-acute care has changed for Medicare beneficiaries from 2000-2015. This blog post summarizes their findings that the percentage of discharges to institutional post-acute care, including skilled nursing facilities and inpatient rehabilitation, increased from 21% in 2000 to 26% in 2015, and that the length of stay in these institutions had increased as well. The increases in post-acute care and length of stay might come as a surprise to those who assumed that payment reform would reduce institutional care. Werner and Konetzka note that the benefit to patients of post-acute care is relatively uncertain, even as its use increases.