Blog Post
Regional and Temporal Patterns in Overuse of Medical Care
Persistent patterns provide insight

Overuse of medical care—the provision of services that can do more harm than good—remains a key driver of waste in our health care system. While most work on this topic has focused on individual overused services, we think it is valuable to conceptualize overuse as a systemic phenomenon, defined as the general tendency of an organization or region to overuse medical services. It turns out that regions and organizations have persistent patterns of overuse, and we’re beginning to understand why.
In our recent work, my colleagues and I map out the distribution of systemic overuse in commercially-insured adults across regions and across time (2011-2015), identifying structural differences in regional health care delivery systems with greater overuse.
To measure systemic overuse, we created an index of 19 low-value service indicators. These “bellwether” services capture 11 unique clinical areas—primary care practice, otolaryngology, radiology, cardiology, neurology, emergency practice, allergy, oncology, urology, physical therapy, and surgery. We applied this index to a large national claims database for adults with employer-sponsored health insurance.
In our first paper, we found that systemic overuse was lower in rural regions of states than in metropolitan areas. Examples of high overusing metropolitan regions include areas in Washington, California, Texas, Louisiana, Florida, New Jersey, and New York. There was relatively little overuse in the central and northwestern parts of the US. These geographic patterns are similar those seen in the Medicare population.
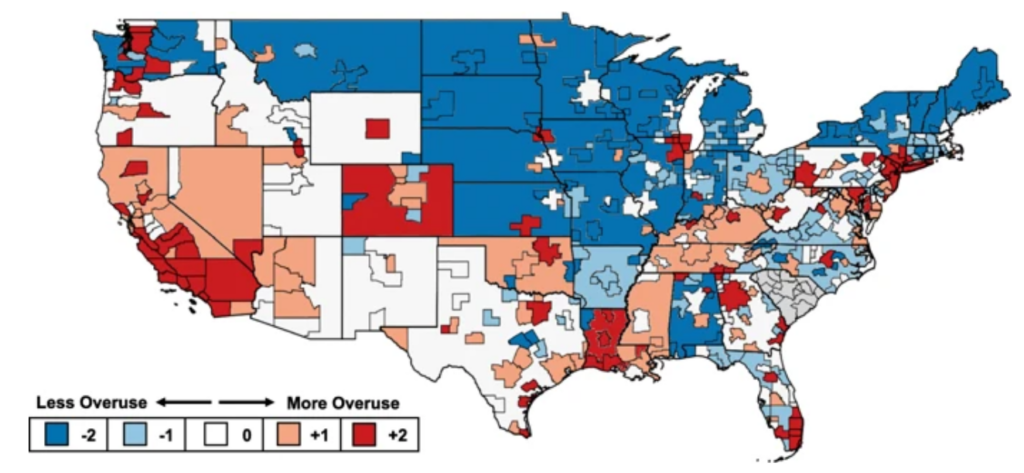
These patterns persisted over time. From 2011 to 2015, the majority of regions remained in the same overuse quintile, making “consistency” the most common phenotype. This was particularly true in the tails—19% of regions were in the top or bottom quintile throughout study duration. The 37 regions that had persistently high rates of systemic overuse support the concept of a distinguishable culture of overuse.
In our latest paper, we found that structural features of the regional health care system related to 1) resource availability, 2) health services configuration, 3) market competition, and 4) clinical customs were associated with systemic overuse. For example, the overall supply of physicians was associated with more overuse, while the supply of primary care providers was associated with less overuse. Again, this finding replicates previous work in the Medicare population.
We found a novel relationship between market competition and systemic overuse: metropolitan areas with a competitive hospital market and an uncompetitive insurer market were associated with more overuse, while areas with an uncompetitive hospital market and a competitive insurer market were associated with less overuse. In addition, we found that a proxy for defensive medicine (the Medicare malpractice geographic price cost index) was associated with systemic overuse. These findings suggest that the differential supply of health care resources can affect practice styles and patterns of wasteful utilization, both across the country and within each state.
By understanding the drivers of health care overuse, we can develop and test more effective interventions to reduce the nearly $100 billion in waste in our health care system. A systematic review of interventions to reduce low-value care found that multicomponent initiatives are more likely to succeed than single component efforts. Because no intervention is likely to suffice on its own, purposeful experimentation is the only way to determine how different strategies can be combined to increase high-value care and decrease low-value care. Looking forward, health system leaders, policymakers, and consumer advocates will likely need to use multiple synergistic levers – at both the individual and systemic level – to increase the likelihood of success.