
Analysis of the Rural Health Transformation Program
Memo: Response to Request for Analysis
Population Health
Blog Post
Most Americans assume that when they go to the hospital there will be an available bed and adequate staffing. Early on in the COVID-19 pandemic, the public and policymakers became acutely aware that hospitals can be overwhelmed. So, what happens to health care delivery when hospitals have more patients than health care personnel and resources available to treat them? Lifesaving care can be delayed.
A recent study in Annals of the American Thoracic Society by LDI Associate Fellow Jennifer Ginestra and LDI Senior Fellows Rachel Kohn, Scott Halpern, Meeta Kerlin, and Gary Weissman explored treatment patterns among ward patients with hospital-acquired sepsis, a particularly high risk group with nearly three times higher mortality than those with community-acquired sepsis. Their findings suggest that timely care for these vulnerable patients may be compromised in the context of high hospital capacity strain.
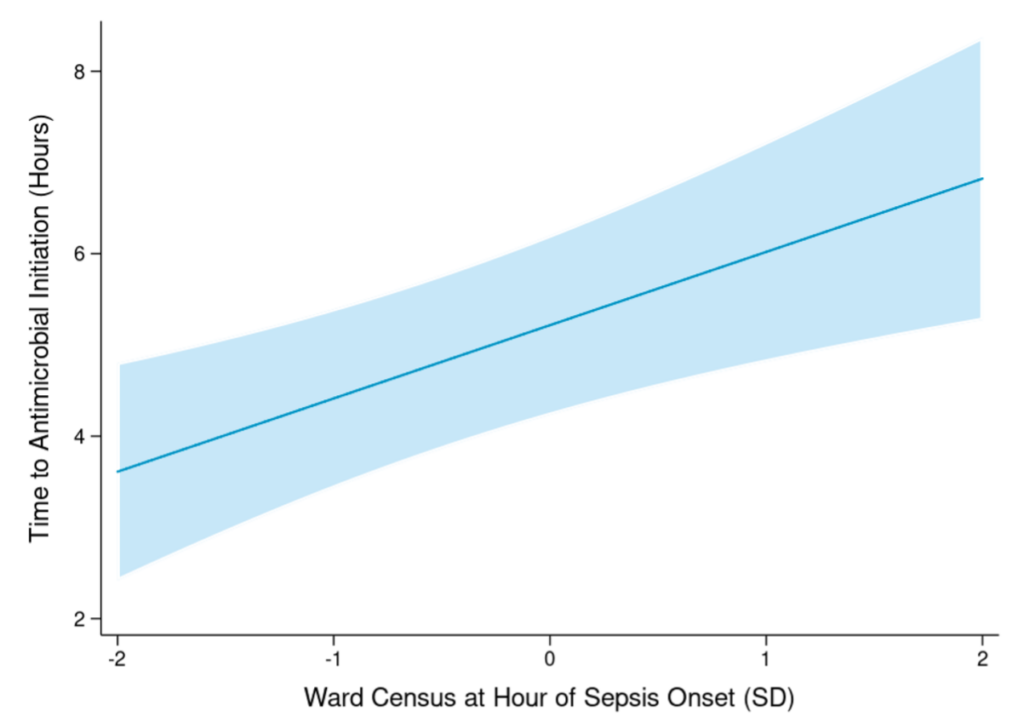
The authors assessed the association between ward census (the number of patients present in each ward at a given time) and antimicrobial initiation among patients with hospital-acquired sepsis. They found that the more crowded hospital wards got, the more treatment was delayed: on average, for every three additional patients present on a given ward, the time to antimicrobial initiation for hospital-acquired sepsis increased by 1 hour. Additionally, only a small percentage of hospital-acquired sepsis patients received antimicrobial treatment within recommended time frames. These findings suggest that treatment for hospital-acquired sepsis infrequently meets quality timing metrics – a problem which may worsen under the pressure of high capacity strain on hospital units.
These data are important as they indicate that a strained health care system can lead to delays in care for some of the highest risk hospitalized patients. To ensure consistent quality care delivery, hospital leaders and policymakers need to consider how to manage capacity strain when patient needs increase – not just during pandemics but in the course of ordinary variation in patient volume.
The study, Association of Unit Census with Delays in Antimicrobial Initiation among Ward Patients with Hospital-acquired Sepsis was published in Annals of the American Thoracic Society on March 21, 2022. Authors include Jennifer Ginestra, Rachel Kohn, Rebecca A. Hubbard, Andrew Crane-Droesch, Scott Halpern, Meeta Kerlin, and Gary Weissman.

Memo: Response to Request for Analysis

Lessons from the Past, Imperatives for the Future

A New Study of a Sample of Facilities Found Half Without Any Behavioral Health Staff

Physicians Were Paid About 10% Less for Visits Involving Black and Hispanic Patients, With Pediatric Gaps Reaching 15%, According to a First-of-Its-Kind LDI Analysis

A New Review Finds Hospital Mergers Raise Prices Without Improving Care, and Urges Regulators to Stop Accepting Quality Claims to Justify Consolidations

Technology Helps Older Adults Stay at Home—But May Delay Necessary Transitions to Higher Levels of Care