
Contradictions That Confuse Federal Food Policies
Announcing Bold New Goals While Crippling the Infrastructure Needed to Achieve Them
Population Health
Blog Post
Hypertensive disorders during pregnancy, such as gestational hypertension and preeclampsia, can lead to significant maternal complications and even death in the months after delivery. In an effort to address this risk and disparities in accessing postpartum care, a program of remote blood pressure monitoring combined with bi-directional text messaging improved rates of postpartum hypertension monitoring, but what about patient outcomes?
A new study published in the Obstetrics & Gynecology by LDI Senior Fellow Sindhu Srinivas and colleagues evaluated the impact of the text-message-based remote blood pressure monitoring program initiated within the first 10 days after delivery. The study aimed to assess its impact on mitigating adverse postpartum clinical outcomes. The researchers also evaluated health care utilization costs among study patients.
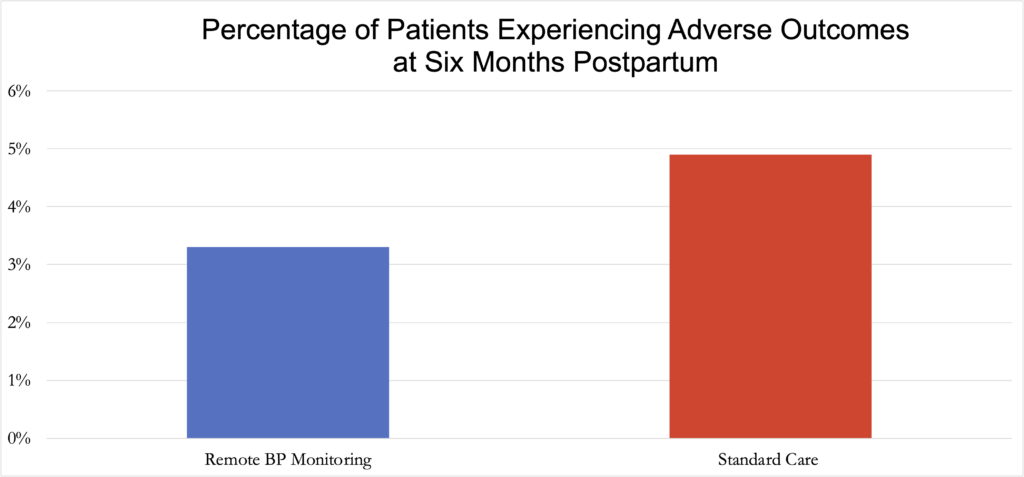
In the six months following delivery, patients enrolled in the remote blood pressure monitoring program were less likely to experience adverse clinical outcomes compared to a matched comparison group of patients who received the usual care. These comparison patients were eligible for the remote blood pressure monitoring program but were treated in other hospitals. Adverse outcomes measured were stroke; disseminated intravascular coagulation; eclampsia; pulmonary edema; kidney injury or liver failure; hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome; heart attack; and heart damage.
Patients enrolled in the remote blood pressure monitoring program were more likely to access necessary treatment and had more cardiology visits than patients in the comparison group. They also had fewer emergency room visits and hospital readmissions, as well as lower total medical costs compared to the patients in the control group. These results remained when the authors compared those receiving blood pressure monitoring to a second comparison group—patients who were not enrolled in the program but received care in the same hospitals as the intervention group, prior to the program being available.
The study adds to our understanding of how remote patient monitoring can drive better patient outcomes and reduce costs, specifically in the postpartum setting. The results indicate that a 10-day remote blood pressure monitoring program, as part of a larger postpartum hypertension bundle of care, reduces maternal morbidity and mortality due to hypertensive disorders of pregnancy up to six months after delivery.
The study, “Association of a Remote Blood Pressure Monitoring Program With Postpartum Adverse Outcomes,” was published in June 2023 (online May 4, 2023) in the Obstetrics & Gynecology. Authors include Adi Hirshberg, Yifan Zhu, Aaron Smith-McLallen, and Sindhu Srinivas.


Announcing Bold New Goals While Crippling the Infrastructure Needed to Achieve Them

Promising New Evidence and What’s Next

From 1990 to 2019, Black Life Expectancy Rose Most in Major Metros and the Northeast—but Gains Stalled or Reversed in Rural Areas and the Midwest, Especially for Younger Adults
A Penn LDI Seminar Focuses on Why They’re Important for the Future

Former Philadelphia Health Commissioner Warns That Gutting the CDC, Undermining Vaccines, and Politicizing Science Will Leave the U.S. Dangerously Unprepared for the Next Pandemic

Rural Parents Had More Emergency Visits and Insurance Loss Than Urban Peers, an LDI Study Shows. Integrated Baby Visits Could Help All Parents Be Healthier