
Black and Hispanic Children Have Higher Death Rates Than White Children After In-Hospital CPR
Equitably Improving Care for Hospitalized Kids Who Experience Cardiac Arrest Requires Hospital-Level Changes, LDI Fellows Say
Blog Post
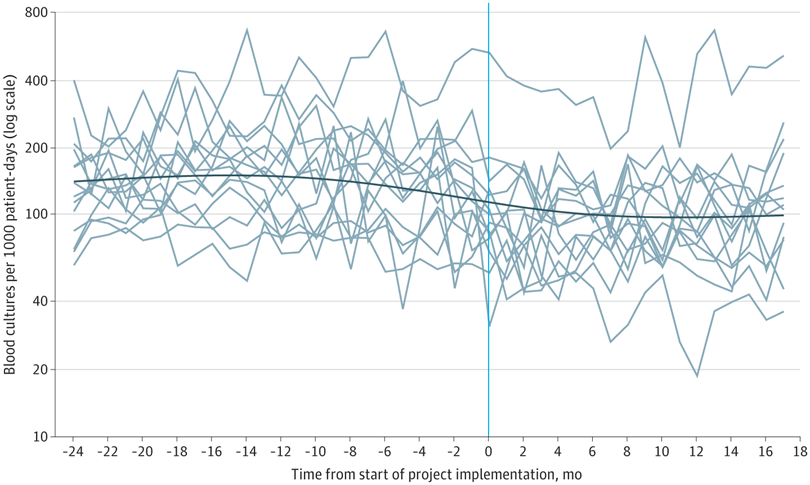
Blood culture tests are commonly overused in the pediatric intensive care unit, a practice that leads to unnecessary antibiotic use and contributes to antibiotic resistance. Optimizing blood culture practices through diagnostic stewardship may reduce unnecessary blood cultures and antibiotics.
In a new study in JAMA Pediatrics, my coauthors and I report on a multicenter diagnostic stewardship intervention designed to optimize and reduce the use of blood cultures for critically ill children. The intervention involved 14 pediatric ICUs—all members of a collaborative called Bright STAR. When we assessed the effects of the Bright STAR intervention in these ICUs after 24 months, we found it reduced blood cultures by 33% and antibiotic use by 13% without changing safety or balancing metrics, such as mortality or sepsis.
How did we do it? We used human factors engineering to understand blood culture practices across the study hospitals, and then we developed site-specific new clinical tools informed by key stakeholder perspectives and unique patient needs. Throughout the project, we assessed elements of both work system factors and quality improvement infrastructure, and we used customized implementation strategies to integrate the clinical tools at each site.
This study points to a promising strategy to change clinical practice, including one of the hardest changes to make—stopping old habits.
The study, “Association of Diagnostic Stewardship for Blood Cultures in Critically Ill Children With Culture Rates, Antibiotic Use, and Patient Outcomes,” was published May 2, 2022, in JAMA Pediatrics. Authors include Charlotte Z Woods-Hill, Elizabeth A. Colantuoni, Danielle W. Koontz, Annie Voskertchian, Anping Xie, Cary Thurm, Marlene R. Miller, James C. Fackler, Aaron M. Milstone, and the Bright STAR authorship group.


Equitably Improving Care for Hospitalized Kids Who Experience Cardiac Arrest Requires Hospital-Level Changes, LDI Fellows Say

Six Studies That Highlight How Losing SNAP Can Raise Food Insecurity and Affect Health
Includes $1 Million in Donations to Meet a Matching Challenge

For Seven Years, Revenue Has Supported Education, Community Projects, and Better Health Outcomes

Government Regulatory Power Wanes as Power Accrues to Courts and Corporations

Temporary Shutdown Losses are Only the Beginning: New Rules Under the One Big Beautiful Bill Act will Shrink SNAP Benefits, and Worsen Food Insecurity for Millions Across the U.S.
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare

A New Call to Action Urges Three Ways State and Local Leaders Can Act To Ban Additives, Improve Food Labels, and Restrict Marketing to Children