Blog Post
COVID-19 Screening Strategies for Repopulating College Campuses
An Evaluation of Five Approaches
As some college and university leaders plan to resume in-person instruction this spring, it is critical to determine the best way to identify COVID-19 cases among students to safely repopulate campuses. However, there is a lack of consensus about the optimal testing strategy to identify the most infections. In a recent study, we evaluated different screening strategies for the fall term and quantified the number of infected students detected with each approach. While each strategy had costs and benefits, strategies incorporating universal laboratory-based molecular testing detected more cases than symptom-based screening alone. Our findings can serve as a guide for college and university leadership as they look to reopen campuses in the new year.
Using data from published literature and the Centers for Disease Control and Prevention (CDC), we completed a decision analysis to evaluate five COVID-19 testing strategies. Many strategies relied on RT-PCR, or reverse transcription polymerase chain reaction—a laboratory-based test to detect the SARS-CoV-2 virus. We used a target population of 20,000 students (a rough estimate of the number of students returning to the University of Pennsylvania campus).
We evaluated five strategies for the onset of a new semester:
- Classifying students with symptoms suggestive of COVID-19 (e.g., fever, cough, and shortness of breath) as infected with COVID-19 without testing
- RT-PCR testing for all symptomatic students only
- RT-PCR testing for all students, performed once upon entry
- RT-PCR testing for all students and a second test seven days later for symptomatic students with a negative first test
- RT-PCR testing for all students and a second test seven days later for all students with a negative first test
Using the baseline prevalence of COVID-19 in the U.S. at the time of the analysis, we calculated the number of true positives (i.e., students with COVID-19 correctly identified as infected), true negatives (i.e., students without COVID-19 correctly identified as uninfected), and RT-PCR tests for each approach (Table 1). We also quantified the number of RT-PCR tests per true positive (TTP).
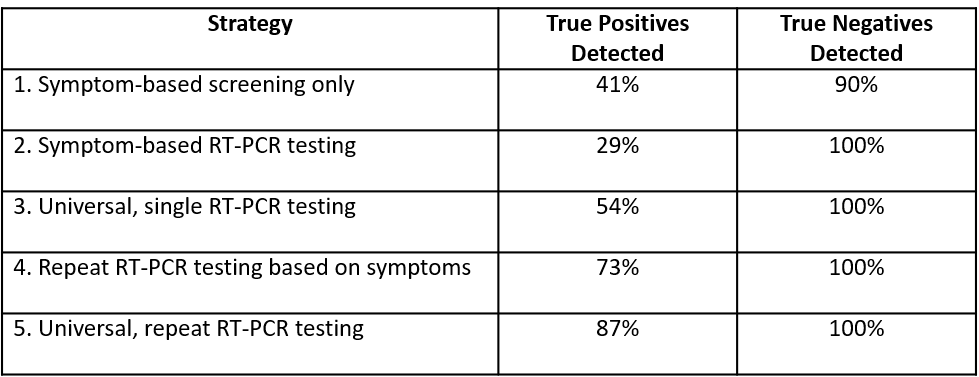
None of the strategies could identify 100% of infected students. Testing all students once and then again seven days later for those who received a negative first test (Strategy 5) detected the greatest proportion of true positives (87%). Relying on symptoms alone without testing (Strategy 1) identified less than half of the true positives (41%), while testing all symptomatic students once (Strategy 2) missed the greatest number of cases, with only 29% of infections detected.
As disease prevalence increased among students, the number of true positives identified increased as well. Strategies that included repeat testing captured more cases but also required more RT-PCR tests. When evaluating the TTP, the repeat testing strategies (4 and 5) dominated. Administering a single test to all students (Strategy 3) was never the best option.
Implications for College and University Leadership

Our results can help guide colleges and universities planning to repopulate campuses during the COVID-19 pandemic. If leaders are uncertain about the baseline prevalence of disease among students, they could adopt a staged approach that begins with a first test upon entry to calculate the prevalence. With this estimate, continued observation of community incidence trends, and knowledge of available resources, leadership could then decide whether RT-PCR testing—and the continued frequency of that testing—would be optimal for the semester.
Of course, a university’s resources and willingness to “pay” will influence the selection of a screening approach. For instance, in the fall, we estimated that a single RT-PCR test might cost $100. If the baseline prevalence of infection on campus is 1%, then the university would have to pay $62,470 (tests per true positive of 624.7 x $100) for each case identified to implement the strategy that detects the greatest proportion of infected students. However, as more tests have become available, this cost has likely decreased considerably since our initial calculation.
If leaders face cost or resource constraints that prevent RT-PCR testing, then we suggest a staged approach that involves initial testing of all students followed by a decision on repeat testing, depending on the baseline prevalence of disease. If there is a low probability of disease among returning students, universities could consider symptom-based screening. Unfortunately, high incidence levels of COVID-19 in the community make this strategy less optimal, so repeat RT-PCR testing (Strategy 4 or 5) would be more favorable.
Effective testing is critical for reducing the risk of outbreaks early in the semester and ensuring the safety of the community. Based on our study, as well as findings from previous research, we recommend that college and university leaders implement repeat RT-PCR testing to more safely repopulate campuses. However, we emphasize that all of the evaluated strategies will still fail to detect some infected students. Thus, relying on COVID-19 screening and testing alone to prevent transmission on campuses will not be successful. An effective mitigation plan for repopulating college campuses safely must also incorporate public health preventative measures (e.g., use of face masks, physical distancing, and promotion of handwashing) and effective contact tracing. These combined strategies can promote the continued safety of campuses and communities during the COVID-19 pandemic.
The study, “Evaluation of COVID-19 Testing Strategies for Repopulating College and University Campuses: A Decision Tree Analysis,” was published in the Journal of Adolescent Health in November 2020. Authors include Amelia Van Pelt, Henry A. Glick, Wei Yang, David Rubin, Michael Feldman, and Stephen E. Kimmel.