
Patients Face New Barriers for GLP-1 Drugs Like Wegovy and Ozempic
Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools
Blog Post
Although Medicaid expansion through the Affordable Care Act has had beneficial effects on coverage, access, and some health outcomes, it has not significantly improved many of the challenges facing a important subgroup of hospitals, known as critical access hospitals (CAHs). We shared our findings in a recent study from me, Rachel Werner, and Karen Joynt published in Health Affairs.
CAHs are important sites of care for rural and other underserved areas, and they have long faced financial and staffing challenges. About one-third of all U.S. hospitals are CAHs, defined as hospitals having fewer than 25 beds, located more than 35 miles from another hospital, or historically deemed to be a “necessary provider” by states. There are more than 1,300 CAHs located across the country, and many of them serve as crucial safety-net providers for rural and other underserved communities:
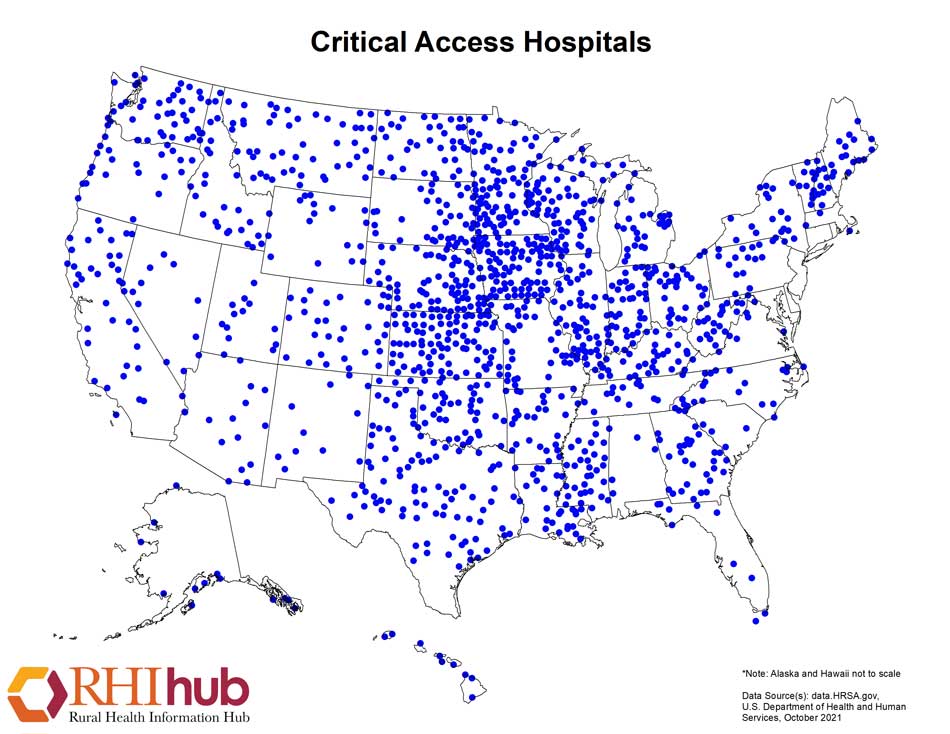
The ACA has been broadly beneficial for rural hospitals with reduced risk of closure in Medicaid expansion states. However, not all rural hospitals are CAHs and not all CAHs are rural. There are many reasons to look at these hospitals separately, given that they are financed differently (reimbursed by Medicare at 101% of costs), have different staffing requirements, and have different quality reporting requirements.
We looked at changes in financial measures, hospital staffing ratios, and quality measures in 1,158 CAHs (648 in Medicaid expansion states and 510 in nonexpansion states) from 2011-2018. We found no significant differential changes in operating margins, uncompensated care, or Medicaid utilization. Similarly, we found no differential changes in physician or nurse staffing, nor in the most commonly reported measures of quality, including patient outcomes and care experiences.
What does this add to our understanding of hospitals and the ACA? Medicaid expansion has done a world of good, but is not a panacea. This may be especially true for rural hospitals facing persistent challenges like declining occupancy and high fixed costs.
The results also highlight the heterogeneity of rural hospitals and communities. About 65% of all rural hospitals are CAHs, and about 85% of all CAHs are rural. Policies that work for some rural hospitals may not work for others.
Beyond Medicaid expansion, states and the federal government are implementing novel strategies designed to bolster rural hospitals and communities. Two exciting demonstrations on the horizon include:
The study, Medicaid Expansion Alone Not Associated With Improved Finances, Staffing, Or Quality At Critical Access Hospitals, was published in the December 2021 issue of Health Affairs. Authors include Paula Chatterjee, Rachel M. Werner, and Karen E. Joynt Maddox.


Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools

A 2024 Study Showing How Even Small Copays Reduce PrEP Use Fueled Media, Legal, and Advocacy Efforts As Courts Weighed a Case Threatening No-Cost Preventive Care for Millions
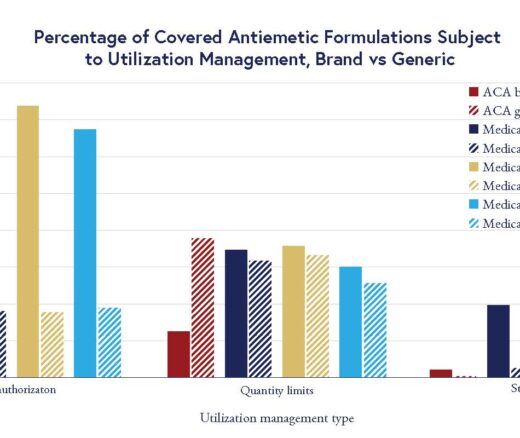
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities