
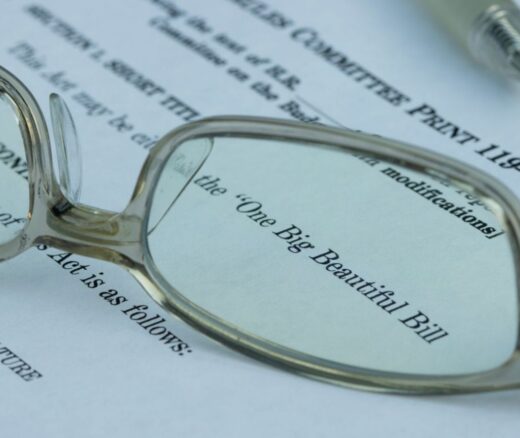
NIH on the Brink: How to Fund Medical Breakthroughs in the Trump–Kennedy Era
With Drastic Cuts on the Table, What’s the Best Way To Fund Medical Innovation – NIH Grants, Prizes, or Bold New Models?
Blog Post

The Affordable Care Act’s Medicaid expansion has been instrumental in improving health outcomes for those who gained coverage and for boosting the finances of providers across multiple U.S. health care sectors. However, the extent to which Medicaid expansion affects economic outcomes among health care workers, especially lower-income workers, is not well understood. These questions are key because, according to co-author and LDI Senior Fellow Paula Chatterjee, “the health care workforce has sizable wage inequality, and lower wage workers are more likely to be in poor health.”
In a recent study, LDI Fellows find that financial benefits from Medicaid expansion in health systems failed to reach the lowest earners. To understand the economic impacts of Medicaid expansion on workers’ annual incomes and their employer-sponsored health insurance, LDI Associate Fellow Sasmira Matta and Senior Fellows Chatterjee and Atheendar Venkataramani studied data from the American Community Survey (ACS), which included more than 1.3 million health care workers in 46 states between 2010 and 2019. They examined data from more than 800,000 health care workers in 30 expansion states and more than 500,000 health care workers in 16 non-expansion states. They focused on differences in outcomes between higher- and lower-income workers, before and after Medicaid expansion, between expansion and non-expansion states.
The researchers found that annual incomes for health care workers in Medicaid expansion states increased overall by slightly more than 2% after expansion relative to workers in non-expansion states. However, these increases were “driven by the highest-earning workers, which included registered nurses, physicians, and managers.” Lower-wage workers did not receive much economic benefit at all.
Financial benefits to health systems might not extend to the lowest earners in those systems. This finding is consistent with known occupational stratification in health care where lack of bargaining power and contract employment can limit gains for these workers.
– Paula Chatterjee, MD, MPH
Lower-income health care workers not only didn’t experience significant increases in annual incomes, these workers were more likely to be enrolled in Medicaid and less likely to receive employer-sponsored health insurance.
Overall, the study findings suggest that Medicaid expansions, which led to increases in financial earnings for health care organizations, “may have benefitted only a subset of workers in ways that can exacerbate economic inequality,” claim the investigators. Therefore understanding the impacts of revenue from Medicaid coverage expansion can help leaders and policymakers proactively address labor inequities within the health care workforce.
In conclusion, Chatterjee says that “low-wage health care workers are among the fastest growing sectors of the economy, are more likely to be women from minoritized groups, and face higher mortality risks. When you take all of this together, our findings suggest a potential mechanism by which health system finances may inadvertently contribute to structural marginalization.”
The study, “Changes in Health Care Workers’ Economic Outcomes Following Medicaid Expansion,” was published on February 27, 2024 in JAMA. Authors include Sasmira Matta, Paula Chatterjee, and Atheendar Venkataramani.


With Drastic Cuts on the Table, What’s the Best Way To Fund Medical Innovation – NIH Grants, Prizes, or Bold New Models?

An Analysis of Penn Medicine Healthy Heart Program Provides Insights

From 1990 to 2019, Black Life Expectancy Rose Most in Major Metros and the Northeast—but Gains Stalled or Reversed in Rural Areas and the Midwest, Especially for Younger Adults.

Findings Suggest That Improving Post-Acute Care Means Looking Beyond Caseloads to Nursing Home Quality
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector

The 2018 MISSION Act Cut Travel Times for Veterans Needing Major Heart Procedures but That Came With More Complications in VA Community Care