Acupuncture Could Fix America’s Chronic Pain Crisis–So Why Can’t Patients Get It?
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use
Blog Post
When a rural hospital closes, it can disrupt both the health care and the economy of a community. The health care sector can supply as much as 10% of the jobs in a rural area. Moreover, hospital closures are a national concern: Of 2,000 rural U.S. hospitals, 150 have closed since 2005, and more than 300 are at risk—a situation exacerbated by the pressures of health care under the COVID-19 pandemic.
Previous studies showed links between hospital closures, lower overall employment, and per capita income at the county level. But are closures a driver or symptom of economic decline? A new study by LDI Senior Fellows Paula Chatterjee and Atheendar Venkataramani, with Penn coauthor Yuqing Lin, shows that hospital closures reflect existing economic downturns.
The researchers used new econometric methods to compare counties with and without hospital closures over time. They analyzed 10 economic outcomes including health care sector jobs, overall unemployment, per capita income, and bankruptcies. The methods and their study design allowed them to determine the relationship between closures and economic conditions in more detail than previous studies.
Chatterjee and colleagues found that of the outcomes they investigated, only health care-sector employment significantly decreased after closures, with a 14% reduction in jobs in counties with a hospital closure, compared to counties without a hospital closure. No other outcomes declined significantly, including overall employment, total jobs, or county population.
Instead, authors note, the story is in the pre-existing trends: In areas with a hospital closure, economies were already declining before the hospital shut its doors. For example, the study findings show declining trends in per capita income, total number of jobs, and unemployment in analyses of up to seven years before hospital closures.
In a 2021 working paper, LDI Fellow Diane Alexander and coauthor Michael Richards, used similar methods and had similar results: Counties with a hospital closure had employment reductions mainly in health care and had pre-existing negative trends such as in the housing market.
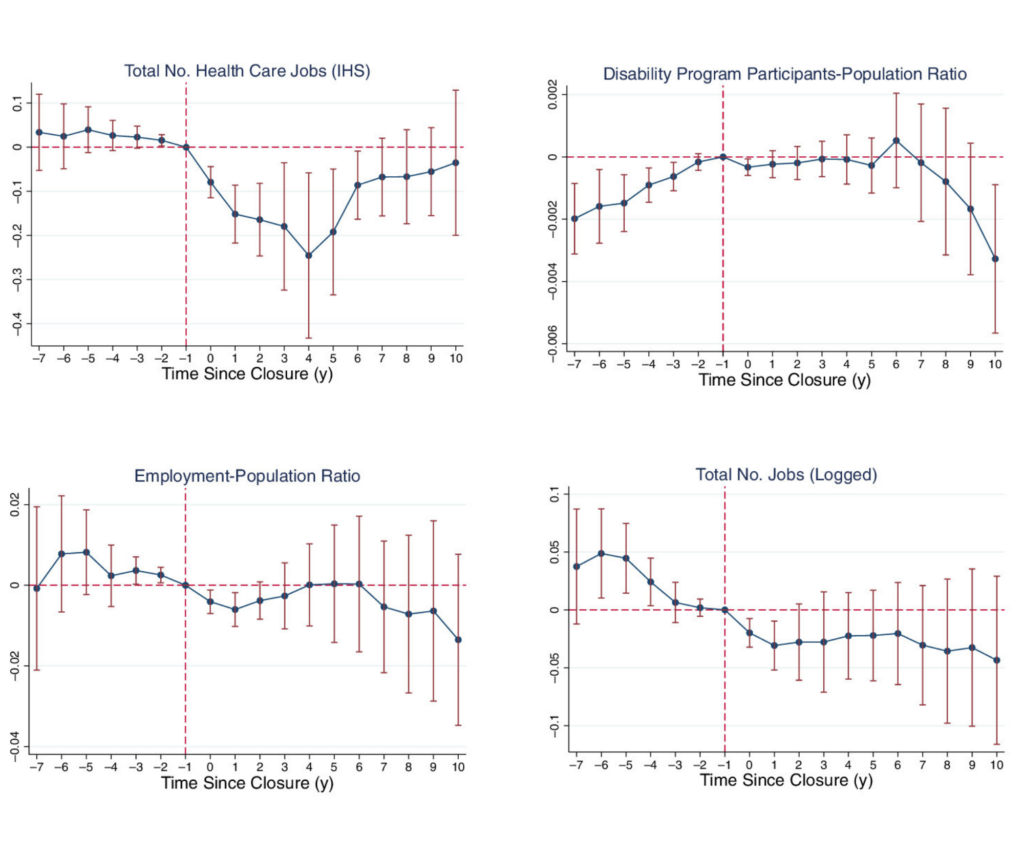
Collectively, these results indicate that upstream economic factors such as unemployment in sectors other than health care and general loss of local investment may lead to low hospital occupancy and poor finances, cascading to closure. Chatterjee and colleagues stress that despite their extensive analysis, current available data are still at the county level. Understanding the local influences and impacts of a hospital closing in a rural area will require more granular data. Fully understanding relationships between hospital closures and the economics of the surrounding area will require sub-county-level data to see interactions and contributions of local factors.
Nonetheless, Chatterjee and coauthors suggest that based on their results, programs and policies that focus solely on stopping rural hospital closures may be ineffective alone. Success at reducing closures may require a broader focus on the hospital’s local community, for example state or federal tax policies to encourage industries in rural markets (e.g., Empowerment Zones). This type of support could boost rural communities in general and positively impact maintaining hospital-based rural health care and the important role it has on the local economy.
The study, Changes in Economic Outcomes Before and After Rural Hospital Closures in the United States: A Difference-in-Differences Study, was published in Health Services Research on April 15, 2022. Authors include Paula Chatterjee, Yuqing Lin, and Atheendar S. Venkataramani.
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare
How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization

Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector