
One Agency’s Maps Are Known For Documenting Redlining
But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says
Population Health
Brief
Cardiovascular disease is the leading cause of death in the U.S. Statins, cholesterol-lowering drugs, are recommended for most people with cardiovascular disease, as they significantly reduce risk of cardiovascular events and related morbidity and mortality. Despite this, many people eligible for statins based on current guidelines do not receive them from their clinician.
Nudges are a promising approach to increase the use of medications such as statins. Typically, nudges are small changes in the way information is framed or in the choices offered to patients and clinicians. Despite the small changes, nudges can have a surprisingly large impact on behavior, including medication prescribing.
In this study, the authors conducted a randomized controlled trial to test the effect of nudges on statin prescribing. The nudges were aimed at patients, at clinicians, and at the combination of the two, and the researchers examined which approach worked best to increase statin prescribing.
When the nudges were aimed at clinicians, statin prescribing increased by 5.5 percentage points compared to usual care. Nudges were also effective at increasing statin use when they targeted a combination of clinicians and patients. In that case, statin prescribing increased by 7.2 percentage points. When the nudges were aimed at patients alone, statin prescribing did not significantly change.
During a 12-month preintervention period, in unadjusted analyses, the rate of new statin prescribing at visits was under 5% in some study arms. With both clinician and patient nudges, new statin prescribing rose to as high as 16% for eligible patients not already taking a statin. The trial had no serious adverse events.
Combining patient and clinician nudges synergistically changed prescribing behavior to increase guideline-directed care. The clinician nudges were automated in a widely used EHR, so they are scalable, pragmatic, and a template for making nudges a standard feature of health care. EHR- based nudges can be add-ons to a delivery system’s EHR
or could become a foundational technology of health IT systems, after rigorous evaluation and in collaboration with EHR vendors.
Digital companies such as Netflix, Amazon, and Facebook effectively nudge users into desired behavior. Automated EHR-based nudges use the same digital strategies to make guideline-based care easy, by presenting the right information to the right person at the right point in the workflow.
This study’s nudge intervention is a model for effective health IT implementation design, involving collaboration between the research team, primary care practices, and health system IT team. The clinician nudge was cocreated with clinicians in an iterative process to ensure uptake and an intuitive user experience.
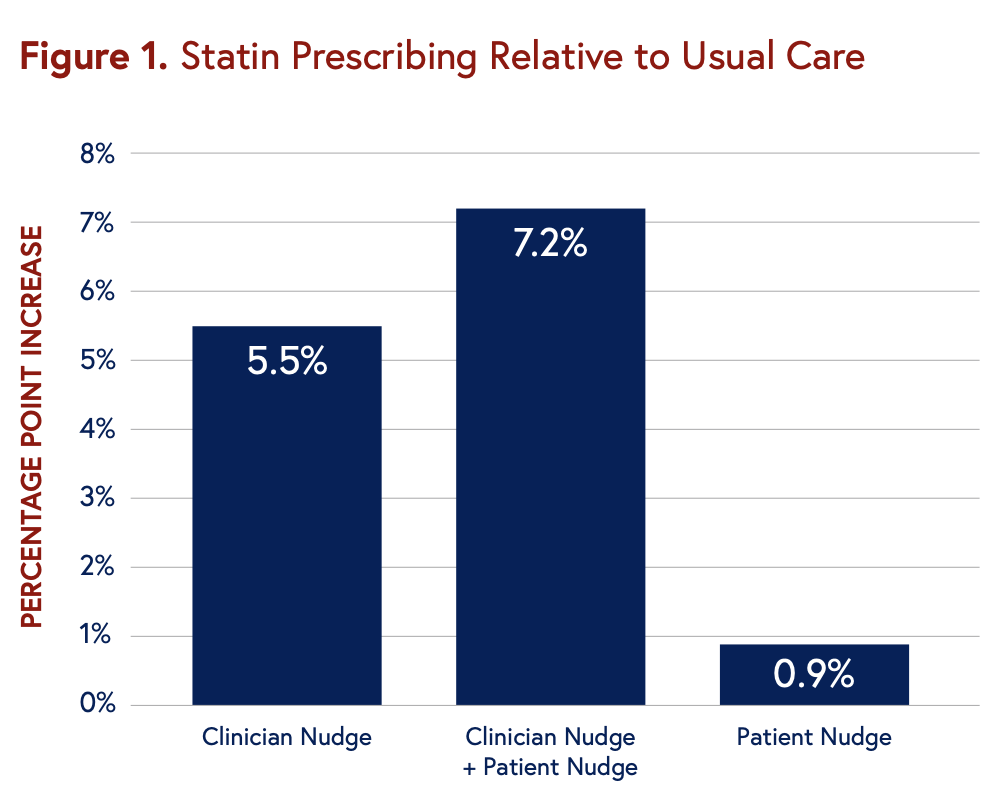
The results indicate that nudging clinicians in conjunction with patients may be most effective in altering behavior. Further more, clinician peer comparison feedback establishes norms and benchmarks for desired behavior, and EHR prompts provide a way to act according to the norms established by peer comparisons.
Additional work in progress includes a qualitative report on patient perceptions of the statin text message nudges.
The authors determined the effect of nudges on statin prescribing by randomizing 28 primary care practices to one of four options: usual care; clinician nudge; patient nudge; or clinician and patient nudges. The primary care practices were part of the University of Pennsylvania Health System, where about 70% of eligible patients had statin prescriptions. The study focused on the remaining patients.
Clinician nudges were implemented in an EHR prompt to order or not order statins for eligible patients during patient visits, plus a monthly feedback report showing statin prescribing of the clinician compared to their peers. Patient nudges were text messages sent a few days before a primary care visit about the risks and benefits of statins with a suggestion to discuss them at their upcoming visit.
Researchers monitored statin prescribing in the randomized practices over the preintervention and six-month intervention period from October 2019 to April 2021. Practices in the study saw a patient group that included 4,131 individuals. Among those, 66% were white and 29% were Black, the average age was 66 years, and 23% had atherosclerotic cardiovascular disease. The primary outcome was initiation of a statin prescription during the visit.
The study, “Effect of Nudges to Clinicians, Patients, or Both to Increase Statin Prescribing: A Cluster Randomized Clinical Trial,” was published on November 30, 2022 in JAMA Cardiology. Authors include Srinath Adusumalli, Genevieve Kanter, Dylan Small, David Asch, Kevin Volpp, Sae-Hwan Park, Yevgeniy Gitelman, David Do, Damien Leri, Corinne Rhodes, Christine VanZandbergen, John T. Howell, Mika Epps, Ann M. Cavella, Michael Wenger, Tory O. Harrington, Kayla Clark, Julie E. Westover, Christopher K. Snider, and Mitesh S. Patel

But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says

Offit and Buttenheim Criticize HHS Placebo Trial Mandate as Unethical, Misleading, and a Threat to Vaccine Confidence

A Penn LDI Virtual Seminar Explores the Latest Trends in Anchor Institution Operations

Neighborhood Perceptions May Also Affect PTSD and Depression Recovery After Serious Injury

A Penn LDI and Opportunity for Health Lab Virtual Seminar Explores Economic Assistance Programs

Testimony: Delivered to Philadelphia City Council