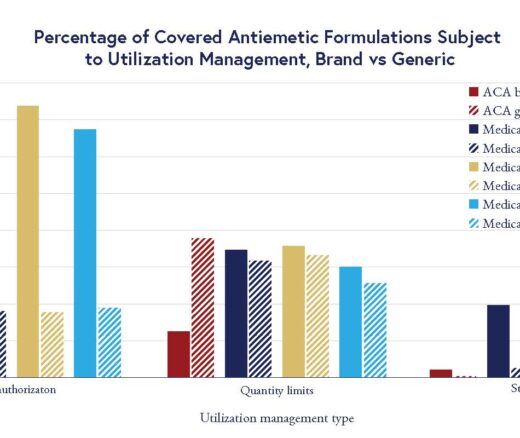
Insurers’ Utilization Management Tools Vary Widely on Anti-Nausea Drugs for Cancer
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea
Blog Post

Major changes are coming to the U.S. organ transplant system. In March, the agency responsible for the U.S. Organ Procurement and Transplantation Network (OPTN) announced plans to modernize the system, including ending a monopoly in place since 1984.
That year, a congressional act gave control of OPTN to a single nonprofit: the United Network for Organ Sharing (UNOS), the only group ever to run the system. Modernization plans include changing to multiple competitive contracts for network components such as operations, oversight, and IT.
LDI scholars agree that the transplant system needs improvements but advise thoughtful consideration of what changes are planned, how they’re implemented, and what the consequences might be. Nonetheless, LDI Senior Fellow Peter Reese said, “There’s lots of impatience with UNOS.”
Problems with the current transplant system include:
Reese said the demand for change now may have been precipitated by fallout from a 2020 policy to share donated livers, kidneys, and other organs over larger regions. That approach disregarded transplant experts who predicted wider organ sharing would lead to longer transport time and more waste, because donated organs degrade with time and centers can get overwhelmed by multiple organ offers. Reese said the policy ignored the poor performance of some nonprofits that obtain organs — called Organ Procurement Organizations — that also underlies regional disparities in transplant access. For example, the procurement organization for New York City has a history of ineffectiveness that contributed to its lower supply of organs, he explained. New York transplant programs advocated for wider sharing, which increased their receipt of livers from nearby states. But the experts turned out to be right: Under the new policy, more livers and kidneys are discarded. Geographic disparities in transplants remain severe.
Additional problems stem from UNOS’s outdated technology. LDI Senior Fellow Nadim Mahmud says clinical transplant coordinators must manually enter, update, and validate much of the patient data that is sent to the national transplant registry, using staff time that could otherwise be spent taking care of patients. Patient tracking could be automated to a greater degree through linkages to electronic health records, Mahmud said. A 2022 U.S. Digital Services report documented other clunky processes and network crashes that introduce dangerous delays that may lead to some organs being discarded.
For nearly 40 years, UNOS has been the sole recipient of the now $6.5 million annual contract to run the OPTN. Although 2022 saw almost 43,000 transplants, that’s not nearly enough to meet demand, leading to long waitlists and deaths. UNOS’s contract is up this year, creating the opportunity for changes. The Biden Administration’s proposed budget doubles OPTN funding to $67 million annually. This covers the modernization initiative plus other programs such as living donor donations. Legislation on the modernization plan is pending. While waiting for Congressional action, the Health Services Research Administration that oversees the network is getting input, including from clinicians and patients.
LDI Senior Fellow Marina Serper advocates for a thoughtful approach to changes. Organ procurement and distribution is “exceedingly complex,” she explained, involving local, state, and federal agencies and multiple steps from donor to recipient. “Thousands of patients benefit from the current system,” she said, “so we need to dig in and see where the problems really are. We have to be careful not to throw the baby out with the bathwater. One solution won’t fix the entire system.”
Mahmud also wants to ensure that changes consider the scope of the problem and the priorities of people such as clinical transplant teams, donor families, and patients. Whenever a transplant policy changes, he says, researchers often find that some inequities are reduced but new ones may arise. “There are always unexpected consequences,” he said. “We need to think about how day-to-day details will change when supplanting the current system.”
An example, Mahmud said, is a potential short-term downside to research. Currently, UNOS collects and cleans all data on donors, recipients, and outcomes, and it releases national data twice yearly. A move to multiple contractors could disrupt this data continuity. “The thought is that more competition might lead to a more efficient system that in the long run could improve transplant allocation equity and reduce costs,” he said. “But with any change, there’ll be a period of pain and adjustment, so disruptions to current processes need to be carefully considered in the transition.”
A process that shouldn’t be disrupted in the organ network overhaul, Mahmud said, is a multiyear plan already underway to promote more equitable allocation of all organs. The “continuous distribution” system is replacing current waitlist prioritization criteria that are organ-specific and rely heavily on a single factor such as medical urgency or predicted post-transplant survival. The new algorithm-based method incorporates and weights multiple patient factors, intending to reduce the unfair exclusion of some patients. Progress towards improving organ allocation should not be halted by transitions to new national registry contracts, Mahmud said.
Reassuringly, the modernization initiative involves developing, testing, and incorporating new system components — such as a data dashboard of organ donations and transplants to increase transparency for clinicians and patients — while gradually replacing existing processes. Reese feels that some critiques of the OPTN are valid, while others might be directed at the transplant community more broadly. He notes that network policies are set by committees that include multiple stakeholders including physicians, patients, social workers, and clergy, as well as public comments.
“In an ideal world, we’ll have much better oversight of OPTN and eventually, a better set of penalties and incentives to improve Organ Procurement Organization performance,” Reese said. “It’s well past time to make some changes to the overall regulatory system for transplant.”

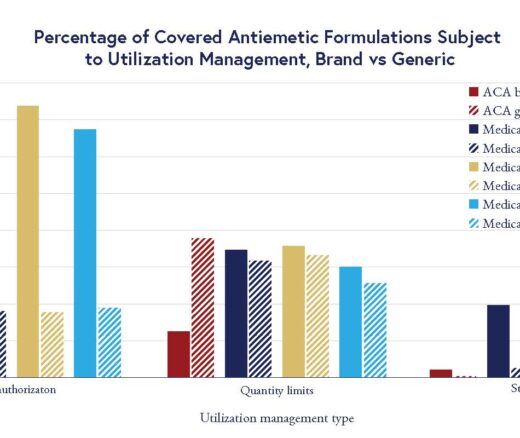
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare
How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization