
Your Emergency Surgery May Rely on Which Surgeon Is On Call
Clinical Reasoning May Lead Two Surgeons to Prescribe Different Treatments to Similar Patients
Blog Post
Last fall, state governments had to prioritize who received COVID-19 vaccinations and booster shots and when. It was complicated. Most states (n=34) used a disadvantage index in their allocation strategy, and nearly half explicitly aimed to advance equity within allocation phases. In a recent BMJ Journal of Medical Ethics study, LDI Senior Fellows Harald Schmidt and Alison Buttenheim, along with their colleagues, studied how the public felt about the government using disadvantage indices.
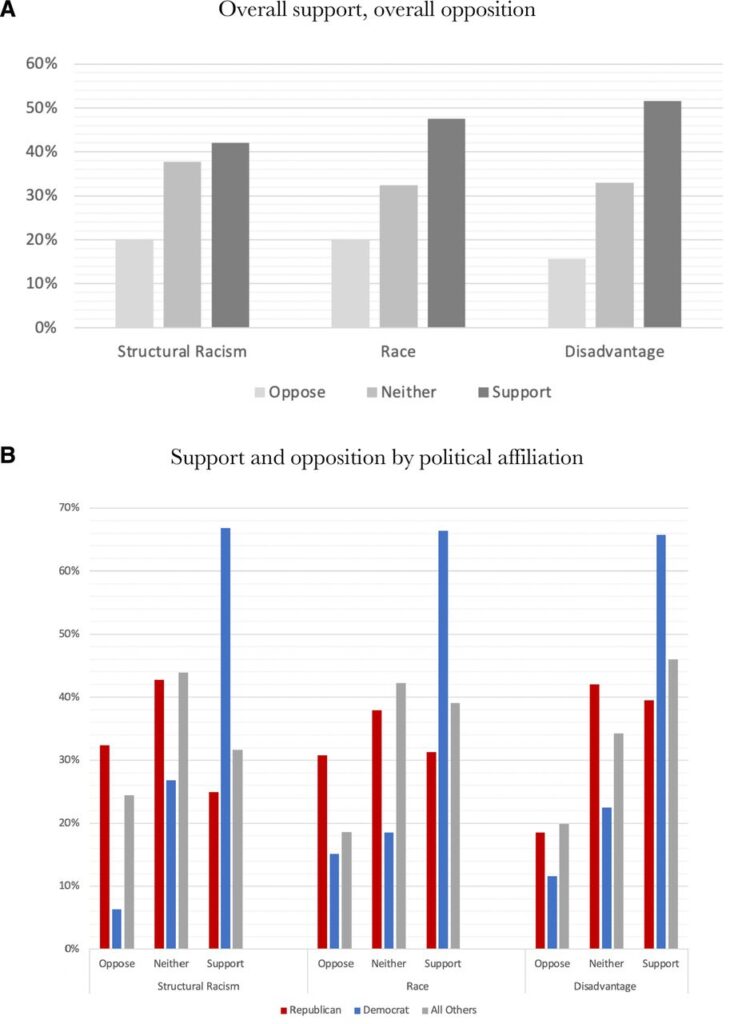
The researchers surveyed a national sample to understand whether support for vaccine prioritization of a disadvantaged population varies if the equity-promoting policy is described as benefitting (1) disadvantaged racial and ethnic groups, (2) disadvantaged racial and ethnic groups affected by structural racism, or (3) disadvantaged groups defined by geographical location (place-based).
Figure A shows that overall support for additional allocations was highest under the place-based description at 51.5% and lowest under the structural racism description at 42.1%. There were big differences in political affiliation. Democrats supported prioritization for disadvantaged groups regardless of how the strategy was described. Republican responders were much less supportive, particularly when the strategy was described as benefitting groups affected by structural racism. It is not surprising to find sharp political divides in the U.S. However, it is important for public health leaders to understand public opinion as they design programs and communicate with the public.
The study, Public Attitudes About Equitable COVID-19 Vaccine Allocation: A Randomized Experiment Of Race-Based Versus Novel Place-Based Frames, was published on August 4, 2022, in the BMJ Journal of Medical Ethics. Authors include Harald Schmidt, Sonia Jawaid Shaikh, Emily Sadecki, Alison Buttenheim, and Sarah Gollust.


Clinical Reasoning May Lead Two Surgeons to Prescribe Different Treatments to Similar Patients

Evidence From More Than 600 Studies Reveals When Financial Incentives Move the Needle—And When They Don’t

Penn LDI Panel Urges Family-Focused Strategy and Stronger Health System Response

Remote Nurses Improved Quality Slightly but Can’t Replace Nurses at the Bedside, a New Study Finds

Washington State’s First-in-the-Nation Insurance Plan Begins Payouts in Mid-2026, and Researchers Will Weigh its Effect on Care, Costs, and the Long-Term Care Markets

Without Pressure From Congress, NHANES — Which Helped Uncover High Levels of Childhood Lead, Nutritional Deficiencies, and Forever Chemicals — Will Cease to Exist