
Methadone Use Rises—But Too Few People Get Opioid Medication
Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
Blog Post
The United States has one of the highest maternal mortality rates in the developed world, and most of these maternal deaths are preventable. Prior studies have shown that hospital staffing significantly influences patient outcomes in other clinical areas, and nursing resources (work environment, staffing, education, specialty certification) may be an important contributor. But little is known about the context in which nurses work on maternity units.
In our recent study in the Journal of Obstetric, Gynecological, and Neonatal Nursing, we examined differences in nursing resources across three different types of maternity units in five regions of the United States. We used the 2016 National Database of Nursing Quality Indicator (NDNQI) survey representing nearly 20,000 nurses who worked in 707 maternity units in 444 hospitals. Our study included nurses working in labor and delivery units, combined labor/delivery and postpartum (LDRP) units, and postpartum units.
We found that the work environment—meaning teamwork, resources, and managerial support—did not vary much across unit types. However, staffing, education, and specialty certification did vary significantly. Notably, most maternity units did not meet staffing guidelines, and staffing was poorest in units in the Southeast. Postpartum units had the worst staffing.
The wide variations in staffing levels suggest that increasing nursing resources may be a system-level target for improving maternity care and outcomes in the United States. In maternity care, one-to-one nursing care is associated with improved birth outcomes. Other research has linked inadequate staffing with more missed care, a problem that is connected to a higher risk of cesarean birth and hemorrhage, poor patient satisfaction, and difficulties establishing breastfeeding, among other issues.
Staffing was but one aspect of work environment that we examined however, improvements in maternal care are sorely needed given the poor U.S. maternal mortality rates. More than half of maternal deaths occur either on the day of delivery or within the first 6 weeks after giving birth. If nurse staffing in maternal units can improve outcomes, hospitals need to find ways to better meet staffing guidelines.
The study, Nursing Resources by Type of Maternity Unit Across Regions of the United States, was published in the Journal of Obstetric, Gynecologic and Neonatal Nursing on March 10, 2022. Authors include Rebecca R.S. Clark, Morgan E Peele, and Eileen T. Lake.



Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
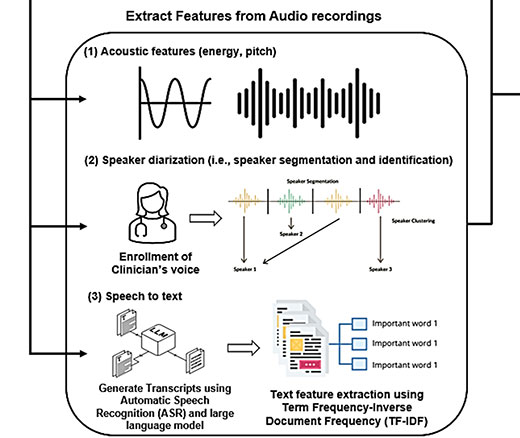
Researchers Use AI to Analyze Patient Phone Calls for Vocal Cues Predicting Palliative Care Acceptance

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

LDI Fellows’ Research Quantifies the Effects of High Health Care Costs for Consumers and Shines Light on Several Drivers of High U.S. Health Care Costs

Comment: Submitted to Centers for Medicare & Medicaid Services

A Licensure Model May Offer Safer Oversight as Clinical AI Grows More Complex, a Penn LDI Doctor Says