Health Equity
Blog Post
How Medical Schools Perpetuate Physician Bias
Reflections and Recommendations
[Editor’s note: In a recent New England Journal of Medicine article, a team of researchers highlighted misrepresentations of race in U.S. medical school courses, and recommended ways to address the systemic racism that produces and reproduces these inaccuracies. In this post, three of the authors—each at different stages of their career—reflect on what they learned about the pervasiveness of the problem throughout medicine, including in their own processes and research].
Jaya: Although it is widely accepted by scholars that race is not a biological category or a risk factor for disease, the use of race is deeply embedded in medical practice and education. Race is a social category—influenced by the social and political landscape—that reflects societal inequalities that produce health disparities along racial lines.
Systemic racism, bias in the health care system, and implicit bias in physicians drive these disparities. Medical education has not yet fully advanced to reflect developments of how race is understood and discussed in the social sciences.
This gap produces physicians who are well-versed in biological sciences, but lack knowledge about their patients’ unique backgrounds and experiences. In response, medical schools have developed curricula in structural competency and cultural humility, where nuanced discussion of race may occur. However, other courses contain inaccuracies that reinforce race-based science.
Kaliya: I gained my first exposure to research through Penn LDI’s Summer Undergraduate Minority Research Program (SUMR). I worked alongside three medical students—Christina Amutah, Adjoa Mante, and Sanjna Surya—to analyze what they were being taught about race in their first 18 months of classes. I was partly responsible for summarizing the problems, providing evidence supporting my summaries, and developing recommendations for medical educators. We analyzed almost 900 lectures from 21 courses in their preclinical curriculum.
Michelle: I joined the research team to help synthesize and contextualize the findings from the content analysis. We identified five key themes that characterize how race is discussed and misrepresented by medical educators: semantics, prevalence without context, race-based diagnostic bias, pathologizing race, and race-based clinical guidelines (Table 1).
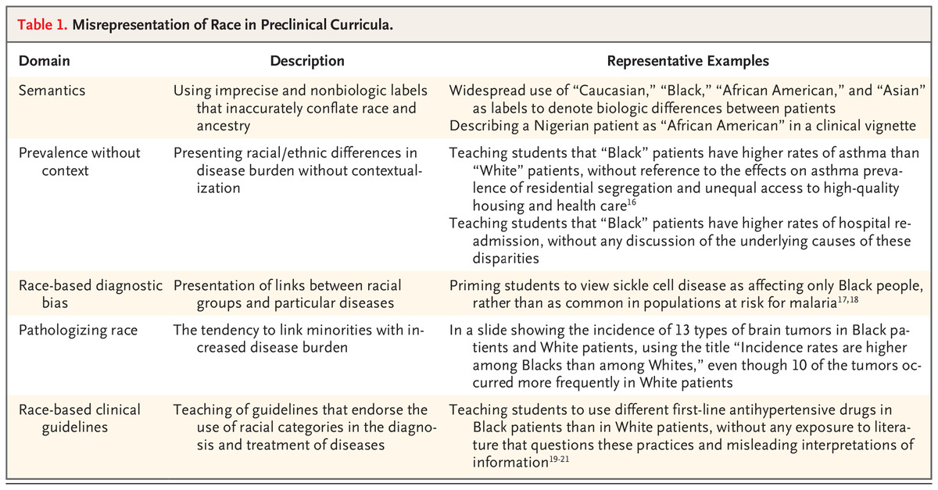
Kaliya: We framed the discussion using common mistakes in the curriculum. A notable example of a mistake in medical education is connecting disease to specific racial groups, implying that the disease does not exist among other groups. For instance, sickle cell disease is associated with Black people and cystic fibrosis is associated with white people. However, members of either group can be afflicted by these diseases, and connecting a disease with one racial group can lead to underdiagnosis in other racial groups.
Another remarkable example is the use of a correction factor when estimating a Black person’s glomerular filtration rate (GFR). Although this adjustment falls under race-based clinical guidelines, it reinforces disparities in kidney transplant referrals. Nevertheless, correcting for race continues to be taught to medical students and used in practice. Our close examination of course slides informed the recommendations we made for medical educators to amend content that misrepresents race (Table 2).
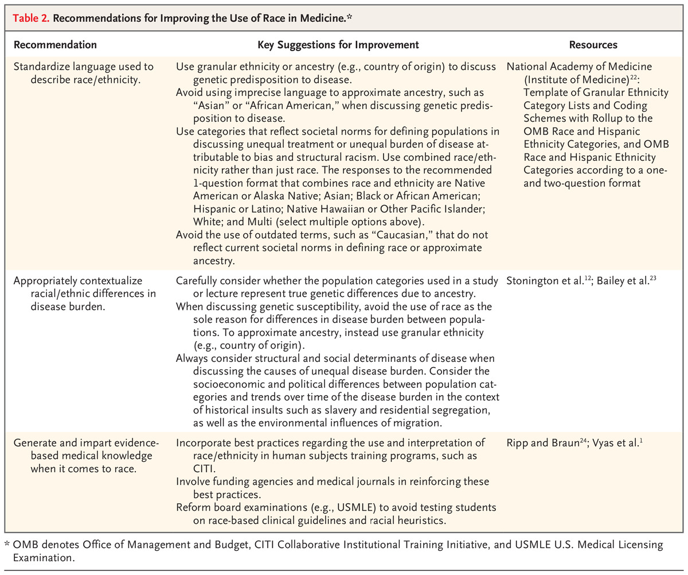
Jaya: In these instances, discussing why we see racial/ethnic differences in disease prevalence will help combat common misconceptions. If we discuss environmental, historical, or societal antecedents to disease among certain racial/ethnic groups, then we dispel the notion that race alone causes such differences.
Michelle: Perhaps most importantly, we saw that these mistakes are common, in part, because structural inequality impacts every aspect of medical education, research, and other knowledge production. We experienced this ourselves in publishing this article. Our team is largely composed of women and scholars of color who belong to groups that have been historically marginalized and underrepresented in medicine. Despite this, we learned after publication that we inaccurately represented Pima communities by neglecting to situate and critique the use of data and narratives about their community in public health.
Ultimately, we committed the very error we cautioned against: we provided inadequate context about the impacts of settler colonialism, Pima/Akimel O’odham struggle and activism, and the sovereignty of their communities. This was an important lesson, and it underscores the pervasiveness of race misrepresentations in our work. It also shows that we have much work to do in medicine, beginning with how we frame and conceptualize knowledge about race, racism, and inequality.
As physicians and scholars, we hold incredible power; learning how to effectively use that power as advocates without recreating the dynamics we work against is a core part of the work.
Jaya: There have been growing calls to dismantle structural racism in medicine. A key first step is to change how we generate medical science and impart medical knowledge related to race. We hope that this framework and the recommendations stemming from our content analysis can help all of us take that first step.



The article, Misrepresenting Race — The Role of Medical Schools in Propagating Physician Bias, was published in the New England Journal of Medicine in January 2021. Authors include Christina Amutah, Kaliya Greenidge, Adjoa Mante, Michelle Munyikwa, Sanjna L. Surya, Eve Higginbotham, David S. Jones, Risa Lavizzo-Mourey, Dorothy Roberts, Jennifer Tsai, and Jaya Aysola.