Blog Post
Improving End of Life Care – Ask the Nurses
Quality care linked to nurse work environment
Everyone wants a dignified death – yet few actually experience one. Despite preferring to remain at home, most older adults spend their final days in hospitals, where they often undergo medical care that neither improves survival, quality of life, nor satisfaction and is often incongruent with their wishes and goals. A new study in the Journal of the American Geriatrics Society describes these problems in end of life care in nearly 500 U.S. hospitals, from the perspective of nearly 13,000 bedside nurses who work in them.

In the study, my colleagues and I found that 58% of nurses rated their hospital’s end of life care unfavorably. More than half of all nurses reported that patients often experience painful or uncomfortable procedures that are not likely to change their clinical outcome. This finding is consistent with growing trends towards aggressive medical intervention in the final days of life, which is widely recognized as inappropriate for terminally ill individuals.
Hospital nurses who care for patients and families at the bedside are well aware of the persistent quality problems in caring for the seriously and terminally ill in the acute care setting. Nurses, by self-selection and education, are highly skilled at caring for the dying, including clinical training in symptom management and comfort care. Yet despite nurses’ capacity as skilled clinicians, their contributions to helping patients achieve a good death are often stymied by organizational constraints including poor working relationships with physician colleagues, lack of authority to practice in their area of expertise, and unmanageable workloads.
In the study, nearly 38% of nurses report being discouraged from discussing alternative care options with patients and families. A similar percentage of nurses say they often disagree with their physician colleagues about end of life care decisions – and feel decisions are not made as a team that includes physicians, nurses, patients, families, and others. In effect, hospitals are failing to capitalize on an already available cadre of skilled end of life care providers – registered nurses at the bedside.
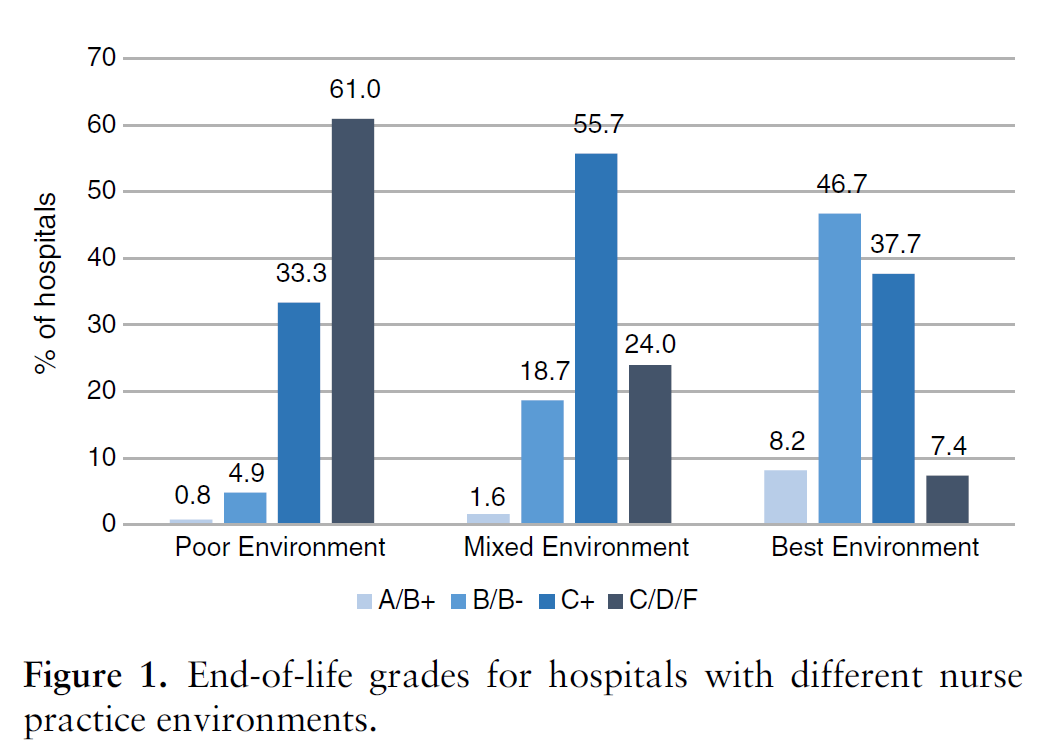
The study found that the best predictor of a hospital’s end of life care quality was the nurses’ practice environment. Nurses in the best environments – those characterized by effective nurse-physician teamwork, where nurses have manageable workloads, the authority to act in their areas of expertise, and a strong voice in hospital decision making – were 55% less likely (than nurses in poor environments) to rate their hospital’s end of life care unfavorably. Improving nurses’ work environments in these areas has been shown to lead to overall improvements in patient care quality and safety – and may also be an intervention for improving the quality of end of life care. As the study shows, even the best hospitals have significant room for improvement in the care they provide to patients at the end of life.
The article, “Quality of End-of-Life Care and Its Association with Nurse Practice Environments in U.S. Hospitals,” was written by Karen Lasater, PhD, RN, Douglas Sloane, PhD, Matthew McHugh, PhD, RN, and Linda Aiken, PhD, RN from the Center for Health Outcomes and Policy Research, School of Nursing, University of Pennsylvania. It appears in Early View in the Journal of the American Geriatrics Society.