
New Parents Put Infants’ Health First, While Their Own Suffers
Rural Parents Had More Emergency Visits and Insurance Loss Than Urban Peers, an LDI Study Shows. Integrated Baby Visits Could Help All Parents Be Healthier
Population Health
In Their Own Words
Cross-posted with permission from Health Affairs Forefront.
[Original Post: Vivek A. Ashok, Laura Bricklin, Anireddy Reddy. Investing In Safety: Reimbursing Safe Firearm Storage Counseling, Health Affairs Forefront, December 9, 2024, https://www.healthaffairs.org/content/forefront/investing-safety-reimbursing-safe-firearm-storage-counseling, Copyright © 2024 Health Affairs by Project HOPE – The People-to-People Health Foundation, Inc.]
“As part of our routine pediatric safety counseling, we ask about firearm safety. Is your child ever near a firearm?”
Since 2019, firearm-related injuries have surpassed motor vehicle crashes as the leading cause of death for children across the United States. In response, many pediatricians have taken on the role of educating families on secure firearm storage. Despite this alarming trend and clear guidance set forth by major medical societies, such as the American Academy of Pediatrics, only a small portion—25 percent to 40 percent—of physicians regularly engage in counseling.
As physicians committed to safeguarding the health and well-being of children from preventable injuries, we need to work collectively to take up this call.
Thankfully, there is momentum for us to do so.
On September 26, 2024, the White House released an executive order allowing states to use Medicaid to reimburse health care providers for counseling families and caregivers on secure firearm storage practices.
State Medicaid organizations must seize this opportunity to encourage clinicians to prioritize firearm injury prevention.
As a general pediatrician and two pediatric intensivists, we witness firsthand the impact of firearm violence on our patients, families, and communities. Authors Reddy and Bricklin, pediatric critical care physicians at Children’s Hospital of Philadelphia (CHOP), care for children with gunshot wounds. Many of these children do not survive, and those who heal in the intensive care unit are left with life-altering injuries and trauma. Some go on to see author Ashok, a general pediatrician, who witnesses the profound impact of these injuries on the mental health of the child, siblings, family members, and wider community. A common refrain runs through our minds: “This could have been prevented.”
In fact, if 20 percent of US households with at least one unlocked gun switched to safe storage, up to 300 youth firearm-involved shootings and up to 135 youth firearm fatalities could be prevented in one year. At CHOP, where we practice, safe storage counseling coupled with a free firearm locking device is the standard of care in our emergency department, three primary care centers, one subspecialty practice, and multiple behavioral health locations, with plans to expand across the enterprise. Similarly, families and caregivers find it acceptable that their health care providers are the ones to counsel. This makes sense—we leverage the trust and rapport that health care providers have with families to promote safe behaviors. Moreover, these conversations have proven effective in improving family and caregiver firearm storage practices.
Beyond saving lives, Medicaid reimbursement for safe storage counseling makes financial sense. In 2020, the total cost of firearm-related injuries and deaths in the US was $493.2 billion, with $78.0 billion attributed to youth firearm injuries. These costs are mostly incurred by taxpayer-funded public health insurance programs—specifically, Medicare and Medicaid. Youth survivors of firearm injury and their caregivers use acute care medical services more and experience higher economic burdens. Christian Pulcini and colleagues studied changes in health care use among 1,800 children before and after firearm injury between 2010 and 2016, identifying an overall increase of $16.5 million in health expenditures. Another study predicted that preventing 11,200 nonfatal youth firearm injuries in 2020 would result in an estimated $62.9 million in population health care savings.
Reimbursement for secure firearm storage counseling is a first step toward prioritizing firearm injury prevention. In addition, state Medicaid organizations should encourage health systems receiving Medicaid funds to provide education to health care professionals on firearm injury prevention. This can include clinician-led secure firearm storage counseling, lethal means reduction counseling, hospital-based violence intervention programs, and universal counseling for firearm injury risk. Medicaid can further incentivize participation in firearm injury prevention education by offering continuing medical education credit for Medicaid-participating clinicians. Lastly, state Medicaid organizations should strongly consider incorporating secure firearm counseling as a performance and quality metric in value-based care models. These approaches facilitate clinician education and are feasible, cost-effective, and aligned with value-based health care.
The medical community works tirelessly to secure healthy futures for their patients and families, and we are asking for help. This policy change supports health care providers in their efforts to prevent firearm injury, ensuring that they have the resources and support to address this issue. Promoting safe storage is not just about preventing tragedies; it is about creating a standard of safety and responsibility for physicians and health systems. It is imperative that states embrace this opportunity swiftly to protect our children and families.
Authors’ Note: Dr. Ashok is funded by National Institutes of Health Training Grant No. T3246118.




Rural Parents Had More Emergency Visits and Insurance Loss Than Urban Peers, an LDI Study Shows. Integrated Baby Visits Could Help All Parents Be Healthier

From Anxiety and Loneliness to Obesity and Gun Deaths, a Sweeping New Study Uncovers a Devastating Decline in the Health and Well-Being of U.S. Children
Before Lawmakers Do Full Legalization, We Must Face the Reality: High-Potency Marijuana Already Harms Kids and Adults Alike

Just Discussing Punitive or Supportive Policies—Even Before They’re Enacted—Can Impact Physical and Mental Health, Especially for Marginalized Groups, LDI Fellow Says
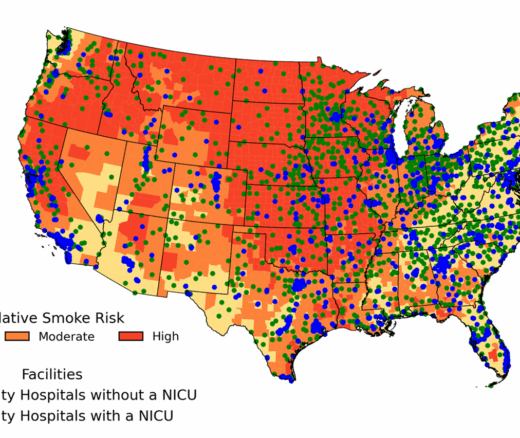
Chart of the Day: New Study Maps Maternity Care Gaps in Smoke-Prone U.S. Counties

But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says